Genetic Variants Linked to Rare but Serious Clozapine Side Effect
Abstract
An international collaboration identifies rare variants in two human leukocyte antigen (HLA) genes associated with agranulocytosis risk in people taking this antipsychotic.
It almost sounds like a Zen riddle: if a medication is effective, but no one uses it, is it really a good drug? That is the conundrum facing the schizophrenia drug clozapine.
“Clozapine is the single most effective antipsychotic available, yet it is used by less than 5 percent of people with schizophrenia,” said Jeffrey Lieberman, M.D., the Lawrence C. Kolb Professor and chair of psychiatry at Columbia University and immediate past-president of APA. “To use this drug in such a limited basis is such a shame.”
The problem lies in the range of potential adverse effects associated with the drug, particularly clozapine-induced agranulocytosis (CIAG), a rare but sometimes fatal loss of white blood cells.
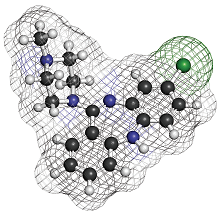
In a major initiative to try and enable safe and widespread clozapine use, Lieberman joined with numerous other researchers worldwide to identify genetic factors that might predispose people to CIAG. As reported September 4 in Nature Communications, this research consortium screened 163 people with CIAG—the largest CIAG cohort ever assembled—and uncovered variants in two genes, HLA-B and HLA-DQB1, associated with CIAG risk.
The two HLA genes make proteins that are part of the human leukocyte antigen complex, a series of proteins on the cell surface that act as a barcode so the immune system can distinguish friendly cells from intruders.
“These are very plausible candidates,” said lead author Fred Jarskog, M.D., a professor of psychiatry at the University of North Carolina School of Medicine and research director at the North Carolina Psychiatric Research Center. “HLA proteins have been tied to numerous adverse drug reactions, and their involvement would be consistent with an immune system-related response like CIAG.”
These findings also confirm an earlier genetic study in a small population of Jewish people with schizophrenia, led by Lieberman, which had first postulated the connection between HLA types and agranulocytosis.
Despite the massive effort, Jarskog cautioned that the relatively small sample size and low frequency of the two risk variants would preclude applying these findings to any diagnostic test. Less than one-third of the CIAG cases carried one of the risky HLA variants, while only 4 percent had both. “So at the moment a genetic test could not provide guidance for more than a handful of people,” he said.
A predictive test would be a long-term goal, as it would overcome two obstacles to widespread clozapine use. To try and detect CIAG as early as possible, people who are prescribed clozapine undergo weekly blood tests to monitor their white-cell counts, a process that burdens both patients and physicians. By identifying a person’s risk, both the threat of CIAG and the need for continual monitoring could be reduced.
Until that time, Jarskog believes, these genetic findings could serve in a different capacity. “We cannot predict CIAG yet, but maybe we can prevent it, or minimize the damage.”
He suggested taking cell samples from people with CIAG who have the risk variants and have experienced the most severe drops in blood cell counts. These cells could be analyzed in a lab setting to try and deduce the molecular mechanism behind the adverse drug response. “If we can figure out how the cells react to clozapine, we might also find ways to block that reaction.”
Both of the risk variants altered the sequence of the protein, and the research group carried out computer modeling that suggested that the subtle protein changes may increase the affinity of clozapine to dock to the HLA proteins, which could affect how HLA “barcode” is read.
The research was supported by the National Institute of Mental Health as part of the American Recovery and Reinvestment Act of 2009. ■
An abstract of “Clozapine-induced Agranulocytosis Is Associated With Rare HLA-DQB1 and HLA-B Alleles” can be accessed here.



