ACA Dependent-Coverage Extension Showing Positive Results
Abstract
Increases in inpatient admissions were significant for both men and women, but were larger for men. Also, the probability of uninsured emergency department visits dropped by 3.9 percent.
Extended dependent coverage for young adults under the Affordable Care Act (ACA) appears to have produced modest increases in general hospital psychiatric inpatient admissions covered by insurance.
And in California, the extended coverage for young adults aged 19 to 25 was associated with a lower rate of emergency visits per 1,000 population in that age group compared with people aged 26 to 29, according to a study published in AJP in Advance.
The ACA requires insurers to permit children to remain on their parents’ policies until age 26. Ezra Golberstein, Ph.D., of the Division of Health Policy and Management at the University of Minnesota School of Public Health, and colleagues from several other institutions conducted a quasi-experimental comparison of a national sample of non-childbirth-related inpatient admissions to general hospitals and California emergency department visits with psychiatric diagnoses, using data spanning 2005 to 2011. Analyses compared young adults who were targeted by the ACA dependent-coverage provision (19- to 25-year-olds) and those who were not (26- to 29-year-olds), estimating changes in utilization before and after implementation of the dependent-coverage provision.
They used three data sources from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project. To study patterns of inpatient hospitalization, they used 2005–2011 data from the National Inpatient Samples (NIS), which are annual random samples of 20 percent of U.S. community hospitals. Golberstein and colleagues complemented NIS data by studying utilization patterns for all inpatient admissions in California’s State Inpatient Database, which includes admissions to specialty mental health or substance use treatment facilities. They also studied emergency department use from 2005 through 2011 in California’s State Emergency Department Databases, which include the universe of emergency department records in the state.
Primary outcome measures were rates of non-childbirth-related psychiatric inpatient admissions, emergency department visits, and the expected primary payer of each inpatient admission and emergency department visit (the last measure allowed assessment of whether the likelihood that services were uninsured or were covered by private insurance changed after the dependent-coverage expansion).
The dependent-coverage expansion was associated with significant increases in inpatient admission rates for all mental illness in the age group targeted by the extension. After stratification by sex, the increases in inpatient admissions were positive and statistically significant for both males and females, but the increase was significantly larger for males. Significant increases for males were found in each psychiatric category, but only depression and psychosis admissions increased significantly more for females among 19- to 25-year-olds compared with 26- to 29-year-olds.
They found further that in California the rate of emergency room visits not leading to an inpatient admission per 1,000 population was 0.45 percent lower among 19- to 25-year-olds than among 26- to 29-year-olds after the coverage expansion.
Finally, after the dependent-coverage expansion, the probability that inpatient admissions and emergency department visits for psychiatric diagnoses were uninsured decreased. The probability that inpatient admissions were uninsured fell 2.9 percent nationally among 19- to 25-year-olds compared with 26- to 29-year-olds, and by 2.8 percent in California. The probability of uninsured emergency department visits in California dropped by 3.9 percent.
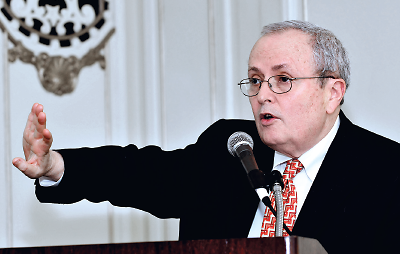
Past APA President Steven Sharfstein, M.D., said the Affordable Care Act is an opportunity for better access to care for people with serious mental illness.
Commenting on the results, past APA President Steven Sharfstein, M.D., said the report would seem to indicate better access to hospital services covered by insurance and—possibly—better access to overall care, given that emergency department use dropped.
“Certainly people with serious mental illness benefit from the ACA,” he told Psychiatric News. “That group is often uninsured either by private or public insurance. The expansion of Medicaid as well as the insurance exchanges enable individuals and families to have access to care in an urgent situation, as indicated by the increase in inpatient admissions, but also early in the process of illness so that there would, potentially, be fewer ER visits, as was found in the study.
“The age period targeted by the dependent-coverage extension is the most vulnerable time for individuals to have a first episode of a serious mental illness, especially schizophrenia,” he noted. “So one would think that by being covered by their parents’ insurance or eligible now for Medicaid, they can get care much more easily than when they were uninsured.”
Sharfstein, who is medical director and CEO of Sheppard Pratt Health System in Baltimore, noted that since the enactment of the ACA, uncompensated care at Sheppard Pratt has dropped by 50 percent. “The main point is that the ACA in combination with parity is an opportunity for access to quality care for people with serious mental illness.”
Golberstein and colleagues noted that as the ACA expands insurance coverage to millions of Americans, it will be crucial to understand the effects of new coverage on patterns of care and spending. “For young adults, a group with significant psychiatric service needs and a group likely to experience large gains in coverage as a result of the ACA, inpatient care for psychiatric diagnoses rose, emergency department use for psychiatric diagnoses fell, and the proportion of hospital-based services that were uninsured dropped after the dependent-coverage expansion,” they concluded. “Future studies will assess whether these patterns will hold as the ACA expands insurance more broadly,” they said. ■
“Effect of the Affordable Care Act’s Young Adult Insurance Expansions on Hospital-Based Mental Health Care” can be accessed here.



