Brain Connectivity Patterns Might Predict Antipsychotic Response
Abstract
Using data obtained from fMRI scans, researchers were able to predict how well patients with acute psychosis would respond to antipsychotic medications with an accuracy of 78 percent.
Finding the most effective antipsychotic for a patient is often a process of trial and error, but research published August 28 in AJP in Advance may have identified a method to identify potential responders before giving them treatment.
The technique involves examining the neural connectivity to and from a region of the brain known as the striatum—an area rich in dopamine receptors that are the targets of antipsychotic medications.
Although previous studies have explored the possibility that physical changes in the brain (e.g. the thickness or volume of certain brain regions) may be able to predict disease onset or the best treatment strategy, most findings suggest that “there is no single lesion that associates with a psychiatric illness,” said Alex Fornito, Ph.D., deputy director of the Brain and Mental Health Laboratory at Australia’s Monash University.
“Pathophysiological changes are subtle and they are distributed throughout the brain,” he told Psychiatric News. “It thus seems natural to conclude that many such illnesses arise from disturbances in the way that different brain regions communicate with each other.”
Deepak Sarpal, M.D., and colleagues at the Feinstein Institute for Medical Research in New York were interested in how brain connectivity patterns might predict treatment response to antipsychotic medications. They used functional MRI (fMRI) to create striatal connectivity maps in a group of 41 first-episode schizophrenia patients. Functional connectivity data were obtained prior to the patients’ participation in a clinical study of risperidone or aripiprazole, and when the study concluded Sarpal’s team compared the connection profiles of responders with nonresponders.
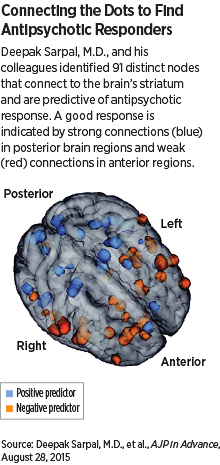
They identified 91 nodes—located throughout the brain—that were functionally connected to the striatum and associated with treatment response. They combined the strength of these connections to develop an overall “connectivity index,” which revealed that antipsychotic drug responders had less striatal connectivity while nonresponders tended to have greater connectivity.
“These results suggest that deficits in the connections between the striatum and other brain regions implicated in psychosis may be the target of antipsychotic medications,” said Sarpal. “By contrast, nonresponders might have an alternate mechanism behind their psychosis that is resistant to the primary functional effects of standard antipsychotics.”
To test how predictive the striatal connectivity index could be, Sarpal and colleagues performed fMRI scans on a group of 40 newly hospitalized patients with acute psychosis. The researchers found that the index could predict a positive response to antipsychotics (in this case measured as at least a 20 percent reduction in symptoms within two weeks) with about 78 percent accuracy.
As a secondary measure, the team also found that the strength of striatal connections correlated with the average hospital stay of these patients.
“This is the first study to validate a predictive fMRI measurement in an independent study group of patients treated with antipsychotics,” Sarpal noted in the article. “The results we found open the door for contemporary ‘precision medicine’ approaches to psychiatry, and more specifically, the use of fMRI scans as important players in the treatment of psychiatric disorders.”
Fornito, who was not involved in this study and has been using brain connectivity scans as potential markers to identify the risk of psychosis and other psychiatric illnesses, applauded the work of Sarpal’s team for successfully validating their discovery. He also noted that the results are consistent with findings from both his group at Monash and a research group at the Institute of Psychiatry, Psychology, and Neuroscience in London.
“We are seeing a general trend in which lower baseline functional connectivity between certain areas predicts better treatment response,” he said.
Trends are not absolutes, however, and Fornito added that considerable work is required to improve the accuracy of these fMRI measurements and demonstrate their robustness among different patients and different settings. Head-to-head comparisons that examine the relative utility of connectivity-based measures for predicting key outcomes relative to more traditional measures like volume changes in specific regions will be important moving forward as well.
“Unfortunately, measures of brain connectivity are intrinsically complex. Changes in cortical thickness or volume can be measured using fairly standard analysis techniques, and these measures are univariate, meaning they index a single property of the brain,” Fornito said. “Measures of connectivity, however, are multivariate, and there is ongoing debate over the best methods for processing the data in order to obtain the most accurate measures of connectivity.”
Nonetheless, Fornito noted there may be much to gain from using fMRI to assess treatment response. “Functional MRI may still be somewhat costly, but surely the cost of a scan far outweighs both the economic cost and personal toll of inadequate or incorrect medication.”
This work was supported by grants from the National Institute of Mental Health. ■
“Baseline Striatal Functional Connectivity as a Predictor of Response to Antipsychotic Drug Treatment” can be accessed here.



