Antipsychotic Nonadherence More Common for Mood Disorders Than Schizophrenia
Abstract
Patients with major depressive disorder or bipolar disorder are also more likely to test positive for marijuana, opioids, and cocaine.
While rates for antipsychotic adherence are most often evaluated in relation to schizophrenia and other psychoses, little is known about adherence rates for such prescribed medicines in populations with nonpsychotic mental disorders.
Contrary to prevailing thoughts, patients with mood disorders (MDD and BD) have higher antipsychotic nonadherence.
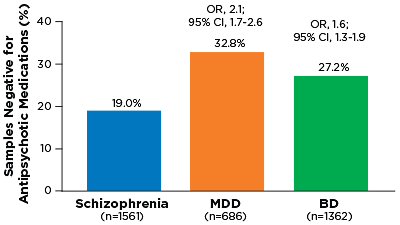
Last month at the American Society for Clinical Psychopharmacology 2015 Annual Meeting in Miami, researchers from Duke University and Ameritox presented results from a study of urine samples that demonstrated that antipsychotic nonadherence is significantly higher in people with major depressive disorder (MDD) or bipolar disorder (BD) than in those with schizophrenia.
The study showed that approximately 33 percent of MDD patients and 27 percent of BD patients were not adhering to their prescribed antipsychotic; for schizophrenia, the nonadherence rate was 19 percent. The findings were obtained from an analysis of over 3,600 unique urine samples.
“These results go counter to conventional wisdom that patients with schizophrenia have the highest rate of medication nonadherence,” said Robert Millet, M.D., the assistant medical director at Carolina Behavioral Care in Durham and a consulting psychiatrist at Duke University.
“Clinicians should appreciate that nonadherence is a significant problem across the spectrum of serious mental illness.”
The analysis also found that a higher percentage of patients with MDD and BD used marijuana, cocaine, and opioids. Approximately 40 percent of MDD patients, 35 percent of BD patients, and 27 percent of schizophrenia patients tested positive for at least one of these substances. Opioid misuse was significantly higher in patients with MDD and BD compared with schizophrenia; cocaine and marijuana use did not differ by disease.
Illicit drug use could be linked with antipsychotic nonadherence, though Michael DeGeorge, Pharm.D., director of medical affairs for Ameritox and Ingenuity Health, noted that there were other differences among the three patient groups. (Ameritox provided funding for this study and performed all of the urine analyses.)
There were demographic differences, for example, with the schizophrenia patients being predominantly male (65 percent) and females making up the majority of MDD and BD patients (60 percent). In addition, the patients in the study were on different types of antipsychotics, with risperidone most commonly prescribed for schizophrenia, aripiprazole for MDD, and quetiapine for BD.
“As a follow-up, we are conducting a multivariate analysis that will take all these factors into account and see if we can identify any trends,” said DeGeorge. “However, since this approach does not involve any direct patient contact, you can never be sure what the actual motivations for the nonadherance might be.”
Still, DeGeorge believes that urine analysis—which has been seeing an uptick in usage—is a valuable tool for psychiatrists, giving them an objective measure of medication use and more confidence to make clinical decisions.
He noted that Ameritox is currently developing more comprehensive reference bases for antipsychotic metabolites, so clinicians can find out not only whether the drug is being taken, but also whether it is being taken properly. ■



