Living Longer, Living Well
Abstract
Two million Americans are now age 90 or older, and this group includes more than 1,000 APA members. This is the conclusion of a two-part series on psychiatrists in their 90s whose active professional lives, community service, and leisure pursuits serve as role models for the rest of us.
A three-times-a-week golfer. Painter of still lifes. Ham radio operator for 50 years.
Many people in their 90s would find any of these pursuits challenging.
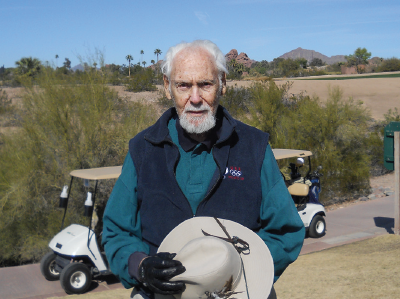
Martin Kassell plays 18 holes of golf three times a week year round. He walks the course. “It’s a beautiful setting, and a great way to exercise,” he says.
Ninety-eight-year-old psychiatrist Martin Kassell, M.D., of Scottsdale, Ariz., relishes all of them. He also still practices and teaches psychotherapy and mentors young psychiatrists.
The Arizona Psychiatric Society (APS) will give Kassell its Career Achievement in Psychiatry Award this month, citing his more than four decades of compassionate patient care, support of peers, leadership, community service, education, advocacy, and clinical excellence. In 2013, APS gave Kassell its Howard E. Wulsin Excellence in Teaching Award. In 2015, he also received APA’s Resident-Fellow Member Mentor Award.
Kassell began his psychiatry training at age 48. Before that, he practiced internal medicine in Philadelphia for 22 years. “My patients would get a little better or a little worse. … I no longer enjoyed my work,” Kassell told Psychiatric News.
A weekend golf partner, a professor of psychiatry at Jefferson Medical College, also in Philadelphia, invited him to visit the psychiatry department. Spending a month there, attending lectures on psychoanalysis and psychotherapy, and observing patient care, Kassell said, reenergized him and refocused his interests.
After training in psychiatry at Jefferson from 1968 to 1971, he directed Jefferson’s community mental health center until 1976. The center served about 2,000 severely chronically mentally ill patients, recently discharged from the state hospital, and others in one of Philadelphia’s most economically deprived communities.
In 1976, thinking ahead toward retirement in a warmer climate, he accepted a position as chief of the psychiatry consultation and liaison service at Phoenix’s Maricopa Medical Center. Two years later, he moved to the Arizona State Hospital, also in Phoenix, eventually becoming its clinical director.
After observing that chronically mentally ill patients often talked more freely with housekeeping personnel than with medical staff, Kassell said, he offered housekeepers training on what to say—and not to say—to patients, and invited housekeepers to team meetings.
He encouraged severely disturbed patients to paint a mural in their dayroom showing a window overlooking a garden and to rearrange furniture to their liking. This project enhanced patients’ self-worth, he said, and gave them a stake in taking care of their surroundings.
He also arranged for patients, their family members or caretakers, and staff to meet informally, have coffee, and chat. One patient who had not left the hospital for 20 years, Kassell recalled, improved enough after such interactions to be able to go out for lunch.
From 1985 to 1994, Kassell directed the psychiatric unit in the Maricopa Durango Jail, a 75-bed facility, and the state’s second largest psychiatric hospital. He incorporated the jail detention staff into the clinical treatment team, improving interaction between detention officers and inmates.
He also arranged to have students at the University of Arizona College of Medicine spend a day at the jail while on their psychiatry rotation, joining staff meetings, interviewing patients, and participating in group sessions. Until 2011, Kassell served as a forensic psychiatrist for the Maricopa County Superior Court.
Kassell lives today in Scottsdale in the house he shared with Evelyn, his wife of 59 years, who died in 2000. His daughter, Stephanie, lives with him. His son, Neal Kassell, M.D., is a professor of neurosurgery at the University of Virginia School of Medicine in Charlottesville.
Teaching and mentoring residents and early career psychiatrists, Kassell said, has been a key source of satisfaction throughout his career.
Today’s emphasis on pharmacotherapy has come at the expense of psychotherapy, a still vital skill, he said. “It’s not adequate to use a pill for everything that’s wrong with a person,” he said. “Psychiatrists need to find out about the person and his way of life.
“A good therapist is one who knows how to listen, not to engage in a conversation to satisfy curiosity, but rather to help the patient,” Kassell said. “A good therapist also has to listen to what the patient is not saying.”
“He’s a wonderful teacher,” noted Payam Sadr, M.D., immediate past APS president and an Arizona APA Assembly representative.
“He keeps up on the latest issues in psychiatry and shares his knowledge at our monthly APS meetings,” said Sadr, who practices in Scottsdale and Phoenix and regards Kassell as a mentor. “He sees every day as a new day.” ■



