Journal Digest
Patients With Suicidal Thoughts Often Not Asked About Access to Firearms

A significant number of patients being treated in emergency departments (EDs) for suicidal thoughts or actions are not asked if they have access to firearms, despite national guidelines urging clinicians to do so, according to a study by researchers at the University of Colorado.
The researchers surveyed 1,358 patients who had been previously admitted to an ED for suicidal ideation or attempts The patients’ charts from these visits were later reviewed to determine whether they had been asked about access to firearms.
Overall, 11 percent of all patients surveyed reported having access to at least one firearm at home. Among 337 patients discharged to home, 55 percent had no documentation of a lethal means assessment by an ED health care provider; 13 percent of those patients had at least one firearm at home.
“Lethal means assessment is important for both overall risk assessment and for safety planning for patients being discharged,” Emmy Betz, M.D., M.P.H., an associate professor of emergency medicine at University of Colorado, said in a press release.
The researchers noted that some clinicians may be reluctant to ask patients about access to firearms because clinicians are unsure if it is appropriate and, if they do ask, what to do with the information.
“It is legal and appropriate to ask about this when it is relevant as it is in the case of suicide attempts or suicidal ideation,” Betz said. “Do it in a respectful, nonjudgmental way, and it will usually be well received. Still, there isn’t a lot of training on this. As a result, we are missing the chance to save a lot of lives.”
Betz ME, Miller M, Barber C, et al. Lethal Means Access and Assessment Among Suicidal Emergency Department Patients. Depress Anxiety. Mar 17, 2016. [Epub ahead of print]
Several Factors Predict Violent Behavior By Mentally Ill People

Results from a meta-analysis in Psychiatric Services in Advance show that alcohol use and recent exposure to violence may predict how likely adults with mental illness are to engage in future violence.
The analysis included information from five studies on more than 2,500 individuals with mental illnesses—including schizophrenia, bipolar disorder, major depressive disorder, and substance use disorder. They were asked questions regarding their exposure to violence (being a perpetrator or victim), alcohol and drug use, psychiatric symptoms, and psychiatric hospitalization. Violent behaviors ranged from pushing and shoving to sexual assault and assault with a deadly weapon and were assessed by the MacArthur Community Violence Screening Instrument. Data were adjusted for age, sex, race, and primary diagnosis.
While current use of alcohol, engagement in violent behavior, and being a victim of violence in the past six months were found to be risk factors predictive of violent behavior six months later, current drug use was not.
“This study provides empirical evidence for three proximal, clinically relevant indicators in the assessment and management of short-term violence risk among adults with mental illnesses,” the authors wrote. “Although clinicians may never be able to answer the public calls for the absolute prediction—and prevention—of violence by adults with mental illnesses, attending to these indicators in clinical practice should assist in the identification of persons [who may be] at heightened risk of community-based violence.”
Johnson KL, Desmarais SL, Grimm KJ, et al. Proximal Risk Factors for Short-Term Community Violence Among Adults With Mental Illnesses. Psychiatric Services. Feb 29, 2016. [Epub ahead of print]
Alpha-7 Agonist Found to Improve Cognition in Nonsmokers With Schizophrenia
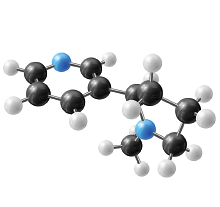
Although current therapies for schizophrenia have been shown to significantly improve positive symptoms of the disorder, none of them noticeably improves cognition. A study recently published in AJP in Advance now suggests that treating patients with schizophrenia with ABT-126—a selective alpha-7 (α7) nicotinic receptor partial agonist—might lead to cognitive improvements, but the medication showed significant effects only in those who were nonsmokers.
Researchers from Cairo University in Egypt and AbbVie Inc., manufacturer of ABT-126, randomly assigned 207 clinically stable patients with schizophrenia to receive 10 mg of ABT-126, 25 mg of ABT-126, or placebo once daily for 12 weeks. The primary efficacy measure was the change from baseline to study endpoint on the MATRICS Consensus Cognitive Battery (MCCB) composite score. Secondary measures included changes in specific domains scores on the MCCB such as verbal learning and working memory.
The researchers found that ABT-126 demonstrated a dose-dependent improvement on cognition that trended toward but did not achieve statistical significance in the 165 patients who completed the trial. Additional subset analyses revealed that nonsmokers taking ABT-126 showed a significant improvement in overall MCCB scores compared with placebo, whereas smokers taking ABT-126 did not. In addition, nonsmokers treated with 25 mg of ABT-126 showed significant improvements in domain scores for verbal learning, working memory, and attention/vigilance.
“No meaningful changes in the severity of schizophrenia symptoms, as measured by the PANSS and its positive and negative symptom subscales, and specifically negative symptoms, as measured by the Negative Symptom Assessment, were observed in the total sample or in subgroups defined by smoking status or baseline level of negative symptoms,” the researchers noted. “These results suggest that the improvements in cognition during treatment with ABT-126 were independent of changes in schizophrenia symptoms and that ABT-126 did not worsen the underlying psychotic illness.”
Haig GM, Bain EE, Robieson WZ, et al. A Randomized Trial to Assess the Efficacy and Safety of ABT-126, a Selective α7 Nicotinic Acetylcholine Receptor Agonist, in the Treatment of Cognitive Impairment in Schizophrenia. Am J Psychiatry. Mar 4, 2016. [Epub ahead of print]
Immune System Protein May Offer Early Indicator of Alzheimer’s
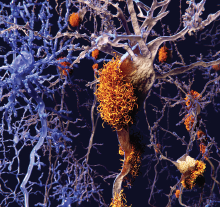
Results from a cross-sectional study published in EMBO Molecular Medicine suggest that the immune system protein TREM2 may offer early clues about patients in the early stages of Alzheimer’s disease.
TREM2 is a protein suggested by previous studies to be involved in neuroprotection when activated. Activation of the TREM2 results in a soluble variant (sTREM2), which can be measured in the cerebrospinal fluid (CSF).
A comparison of the levels of sTREM2 in the CSF of hundreds of people with varying degrees of cognitive impairment associated with AD revealed sTREM2 to be highest in patients with mild cognitive impairment; sTREM2 levels were lowest in patients with AD-related dementia.
“Our data demonstrate that CSF sTREM2 levels are increased in the early symptomatic phase of AD, probably reflecting a corresponding change of microglia activation status in response to neural degeneration,” the authors wrote. ■
Suárez-Calvet M, Kleinberger G, Araque Caballero MÁ, et al. sTREM2 Cerebrospinal Fluid Levels Are a Potential Biomarker for Microglia Activity in Early-Stage Alzheimer’s Disease and Associate With Neuronal Injury Markers. EMBO Mol Med. Mar 3, 2016. [Epub ahead of print]



