Free Practice Support Available Through Transforming Clinical Practice Initiative
Abstract
Psychiatrists are encouraged to take advantage of free training in collaborative care and prepare for changes coming in the delivery and payment of mental health care.
In September 2015, APA was awarded with up to $2.9 million over four years to serve as a Support and Alignment Network in the Centers for Medicare and Medicaid Services (CMS) Transforming Clinical Practice Initiative (TCPI). TCPI is a large national initiative that provides $685 million to 39 national and regional health care transformation networks and supporting organizations to support practice transformation through nationwide, collaborative, and peer-based learning networks.
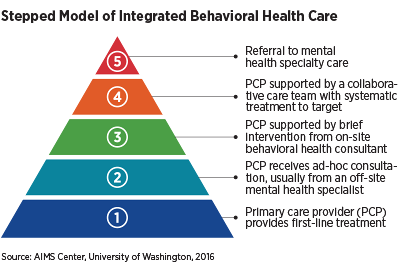
APA is working toward two goals through TCPI: (1) to train at least 3,500 psychiatrists in integrated care over the next three and a half years and (2) to connect psychiatrists with one of the 29 Practice Transformation Networks (PTNs) participating in the initiative.
PTNs are designed to provide on-the-ground support and technical assistance for clinicians as they prepare for alternative payment models and practicing in a value-based world. This support is especially important in helping clinicians prepare for the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) as Medicare increases its rewards to clinicians for participating in new models of care that emphasize value over volume. PTNs provide resources to assist physicians to be successful in new payment models at no cost and no risk to their practice.
Here are a few examples of how PTNs are supporting psychiatrists across the country:
The Care Transitions Network for People With Serious Mental Illness in New York was designed specifically to support clinician practices that serve people with serious mental illness. The network provides individualized practice transformation support with no fees attached, clinical consultation by psychiatrists and internists on evidence-based practices, and incentive payments for meeting certain milestones. Its technical assistance is designed by and for clinicians who know what it is like to practice in the tumult of New York state.
“The road to value-based payment models is fraught with uncertainty but, nonetheless, it is the road ahead of us,” stated Linda Rosenberg, president and CEO of the National Council for Behavioral Health. “The Care Transitions Network is eager to support psychiatric practices to navigate this new terrain and achieve the goals of better patient care and outcomes while also retaining solid financial footing.”
The Rhode Island Quality Institute is a Practice Transformation Network in Rhode Island that provides psychiatric practices with individualized practice transformation support with no fees charged to clinicians. Technical assistance by its trained and dedicated staff helps to prepare clinicians for value-based reimbursement models by providing quality improvement tools and coaching.
CEO Laura Adams stated, “With the recognition of mental health and physical health as inseparable, supporting psychiatric practices in their efforts toward the Triple Aim of better health, better health care, and lower costs is critical if we ever hope to achieve the potential of health care as it should be.”
The Colorado Practice Transformation Network is a public and private partnership providing tools and support to clinicians statewide through TCPI. It is enthusiastic about APA’s participation because behavioral health integration is crucial to the state’s model of practice transformation.
Jacqueline Calderone, M.D., a psychiatrist at the Helen and Arthur E. Johnson Depression Center at the University of Colorado School of Medicine, stated, “The collaborative care model of TCPI is an evidence-based path to leveraging the expertise of psychiatrists, allowing us to impact more patients without having to engage directly with each patient. “
The 29 PTNs cover all 50 states, and many of them are still recruiting psychiatrists for their networks. Learn more about PTNs in your region and complete the online integrated care training on APA’s website or contact [email protected]. Free training will also be available at IPS: The Mental Health Services Conference, which is being held in Washington, D.C., from October 6 to 9. Registration information can be accessed here. ■
This article is supported by Funding Opportunity Number CMS-1L1-15-002 from the Department of Health and Human Services, Centers for Medicare and Medicaid Services. The contents provided are solely the responsibility of the authors and do not necessarily represent the official views of the department or any of its agencies.



