UMass Researcher Turns Idea Into a Nationally Recognized Program
Abstract
MCPAP for Moms offers coordinated psychiatry consults to OB-GYNs to help better prepare them to assess and manage perinatal mental health.
During her psychosomatic medicine fellowship at Brigham and Women’s Hospital in Boston, Nancy Byatt, D.O., M.B.A., had the opportunity to work as a perinatal psychiatrist at an obstetrics and gynecology (OB-GYN) clinic.
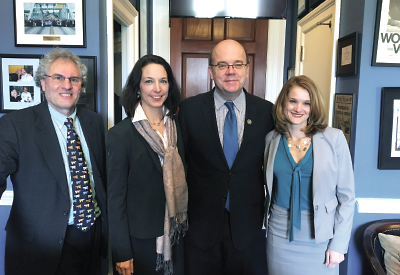
From left: John Straus, M.D., Tiffany Moore-Simas, M.D., U.S. Rep. Jim McGovern (D-Mass.), and Nancy Byatt, D.O., M.B.A., gathered in Washington, D.C., to discuss how to expand the Massachusetts Child Psychiatry Access Program for Moms into other states.
As she learned first-hand just how common depression is among new and expectant mothers, she found herself questioning how psychiatrists could ever effectively handle the burden.
“It also really struck me that the OB-GYNs, who saw these women regularly, wanted to help,” Byatt said. “But, they felt they didn’t have the training to provide adequate care.”
Byatt saw this as a missed opportunity. After finishing her fellowship and taking an academic position at the University of Massachusetts Medical School in Worchester, she began to develop a model that could leverage the OB-GYN community to provide much-needed mental health care to pregnant and postpartum women.
What followed was a whirlwind period where a modest grant proposal would lead to a statewide initiative and a successful program—MCPAP for Moms—that would eventually find its way into federal legislation.
Research Interests Dovetail With State Priority
It all began in early 2013 when Byatt applied for a “K award” (NIH grants aimed at early stage investigators to help them establish a research program) to fund a pilot program she called PRISM (for PRogram In Support of Moms). The program aimed to train OB-GYNs on how to screen and diagnose patients with depression, monitor patient progress, educate them about the benefits and risks of antidepressant therapy during pregnancy and nursing, and connect OB-GYNs with psychiatrists.
A few years prior, the state legislature of Massachusetts formed a commission that was charged with coming up with a statewide initiative to address postpartum depression, with an emphasis on screening.
“The commission was pushing hard for mandatory depression screening for new mothers, but I thought we shouldn’t do it when we had nothing to offer the women who screened positive,” said Tiffany Moore-Simas, M.D., M.P.H., an OB-GYN at the University of Massachusetts Medical School, who served on the state’s Postpartum Depression Commission.
Moore-Simas also happened to be collaborating on research with Byatt. “I knew she was working on a K award on this topic and thought that it would be good for the commission to hear her ideas.”
Byatt agreed that something like PRISM might be able to help women with depression to connect with services, but the project was still too preliminary for any large-scale implementation.
However, the state already had an existing and effective collaborative program known as the Massachusetts Child Psychiatry Access Program (MCPAP), which provided quick access to psychiatric support for pediatricians and family doctors. She realized that by incorporating elements of PRISM into MCPAP, she might be able to make an extension of the program aimed at new or expectant mothers.
She worked closely with pediatrician John Strauss, M.D., the founding director of MCPAP, to develop a strategic plan for the extension, known as MCPAP for Moms. In November 2013, she was notified that the MCPAP for Moms program would be funded (which was just two months after her K award was also funded). MCPAP for Moms is funded by the Massachusetts Department of Mental Health.
“The only hitch was we only had eight months to fully develop and conceptualize our program,” Byatt said.
Byatt was hardly deterred. “I had already spent years thinking about integrating depression and obstetric care [for the PRISM proposal], just on a smaller scale,” she said. After Byatt met with focus groups and received feedback from providers and staff at different clinics, the MCPAP for Moms was launched in July 2014.
MCPAP for Moms Sees Early Success
MCPAP for Moms connects OB-GYN clinics with perinatal psychiatrists who provide on-site training on how to detect, assess, and manage depression and other mental health concerns in pregnant and postpartum women. All of the assessment guidelines, screening tools, and treatment algorithms are also available online for the clinicians to use.
Once enrolled, an OB-GYN provider can also call a MCPAP for Moms care coordinator if additional assistance is needed; the coordinator will link the provider with an on-call psychiatrist for an immediate telephone consultation about the patient.
The consults between an OB-GYN and MCPAP for Moms psychiatrist are meant to be educational and develop the provider’s knowledge base. Byatt emphasized that the consulting psychiatrists do not initiate treatment—they make recommendations and let the OB-GYN choose the treatment they feel is best for the patient. For particularly difficult cases, one-time, in-person consults between a patient and psychiatrist can also be scheduled.
It’s a simple approach that has produced impressive results; two and a half years after launching, MCPAP for Moms has enrolled over 100 OB-GYN practices (more than half of the OB-GYN practices in the state) and served over 2,400 women.
Beyond the number of women served, there is also evidence that the women are getting better, Byatt said. “Some of our latest pilot data show that patients who were served by practices that are enrolled in MCPAP for Moms improved by five points on the EPDS [Edinburgh Postnatal Depression Scale].”
Many individuals and groups have taken notice, including APA, which recently awarded MCPAP for Moms with the 2016-2017 Psychiatric Services Gold Achievement Award for academic programs.
MCPAP for Moms also attracted the attention of U.S. Rep. Katherine Clark (D-Mass.). Clark later sponsored a bill known as the Bringing Postpartum Depression Out of the Shadows Act, which aims to provide funding to states “to establish, expand, or maintain culturally competent programs for screening and treatment of women who are pregnant, or who have given birth within the preceding 12 months, for maternal depression.”
Rep. Clark, together with James S. Gessner, M.D., president of the Massachusetts Medical Society, and Maryanne C. Bombaugh, M.D., chair of the Massachusetts section of the American Congress of Obstetricians and Gynecologists, wrote of the impact of MCPAP in an opinion piece in STAT in January: “In the first 18 months of the MCPAP for Moms program, more than 1,100 women were screened and treated for postpartum depression. We believe that the Bringing Postpartum Depression Out of the Shadows Act will allow this successful state program to be scaled nationally and, in doing so, positively affect the well-being of women and their families across the country.”
The Bringing Postpartum Depression Out of the Shadows Act was eventually folded into the comprehensive 21st Century Cures Act, which was signed into law in December 2016 (Psychiatric News, January 6).
“This is beyond what I ever would have imagined when I first started my grant application just a few years ago,” Byatt said. “But it would not have been possible without the support of so many parties, from the leadership at MCPAP, our program director Kate Biebel, the members of the commission, my mentors and colleagues at UMass, and especially Tiffany and the OB-GYN community, whose eager buy-in was essential.”
“For mentors like myself, seeing research ideas germinate into nationally recognized programs is extremely satisfying,” said Douglas Ziedonis, M.D., chair of the psychiatry department at the University of Massachusetts Medical School, who advised Byatt on her K award application.
“Equally fulfilling has been witnessing the transition of Byatt from gung-ho clinician into a leader in the field of postpartum depression,” he added.
Ziedonis added that Byatt’s journey highlights the wide range of research options that can align with a clinician’s passion.
“It’s not just test tubes and statistics,” he said. “For Byatt, there were opportunities in implementation science that helped build her program.” ■
More information on MCPAP for Moms can be accessed here.



