New Report Highlights Need for Integrative Adolescent Care
Abstract
Understanding which physical health conditions are associated with depression is important to aid in prevention efforts and timely identification of at-risk populations.
A report from the Substance Abuse and Mental Health Services Administration (SAMHSA) sheds new light on the complex interaction between mental and physical illness among adolescents.
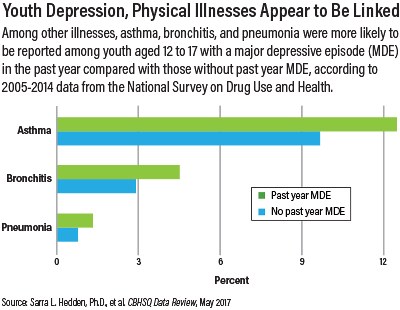
Authors Sarra L. Hedden, Ph.D., and colleagues from SAMHSA’s Center for Behavioral Health Statistics and Quality analyzed 2005-2014 data from the National Survey on Drug Use and Health regarding the association between major depressive episode (MDE) and several chronic and acute medical illnesses.
Among many findings, the data showed that asthma, diabetes, bronchitis, pneumonia, and obesity (in females) were significantly associated with MDE in the past year. Adolescents with past year MDE were also much more likely than those without to report fair or poor overall health versus good or excellent overall health. The findings were mostly consistent across age, gender, socioeconomic, and racial/ethnic groups.
The data were cross-sectional and therefore do not indicate directionality or prove causation, but the point is to highlight the associations and the need for integrative approaches to management, according to study co-author Rachel Lipari, Ph.D.
“It’s just a single point in time, but it is a very large, nationally representative survey. We’re looking at associations between physical and behavioral health that we see in clinical settings, but we’re now able to replicate these relationships on a national level.”
Added co-author Lisa Rubenstein, M.S., “We’re focusing on the importance of integration between primary care, specialty care, and behavioral health. The way we see the important usage of these data is to have tailored messages. If you’re taking care of people with depression, you might have better behavioral health outcomes if you partner with the primary care providers.”
And for primary care providers, Rubenstein said, the goal is to promote depression screening among patients with asthma or diabetes, or obese females. “Until we can do full integration, this really needs to be addressed,” she noted.
Washington, D.C., child psychiatrist Adair Parr, M.D., called the report’s cross-sectional nature “a limitation,” but she also sees it as an important reminder for psychiatrists to be mindful of any diagnosed physical illnesses and to be on the alert for incident medical conditions in existing patients with depression or other major mental illnesses.
For children with a chronic condition, she said, questions to consider asking them and their families include “How are they managing that in addition to their emotional problems? What are their coping strategies? What is the family support like?”
Lipari and her colleagues plan to delve further into the data using advanced statistical techniques to tease out more information about the identified relationships.
Report Part of Larger Effort
The report is part of a multi-pronged SAMHSA initiative to promote optimal integrative care models. The agency’s annual National Children’s Mental Health Awareness Day in May focused on the importance of integrating behavioral health and primary care for children, youth, and young adults with mental and/or substance use disorders (Psychiatric News, June 2).
The main event was held in Washington, D.C., while related events and activities were held in other cities nationwide. Several panels examined models for fully integrated health care and how best to facilitate communication among providers.
Parr was among the panelists at the D.C. event (Psychiatric News, August 4). She described her recent work in setting up a collaborative care psychiatry program within a large private pediatric practice. She reviews patients’ electronic medical records and makes recommendations to the pediatricians via chart notes. For patients who need greater assessment and intervention, Parr sees them in person.
“It’s kind of a hybrid of co-location and the collaborative care model,” she explained, adding that the setup overcomes both the geographic and financial barriers in usual-care models. “Everyone is challenged by communication, … and often you’re not getting paid for that time.”
To aid in promoting such endeavors, SAMHSA has begun partnering with professional societies and organizations that specialize in the medical conditions cited in the report, including APA, the American Academy of Pediatrics, the American Academy of Family Physicians, the American Diabetes Association, and other federal agencies, to work on an integration campaign.
A meeting is now being planned to examine the various evidence-based integrative models, including co-location, full integration, and telehealth for remote areas that lack mental health professionals. “That hasn’t been done before,” Rubenstein said. “It’s the application of the data that’s new and exciting.” ■
“Comparison of Physical Health Conditions Among Adolescents Aged 12 to 17 With and Without Major Depressive Episode” can be accessed here.



