Data Show Strong Link Between Depression, Mortality
Severe depression is as dangerous to elderly people as are cancer, heart disease, high blood pressure, and emphysema, according to a new study.
“There is a very strong link between depression and mortality when the depression is severe,” said Jurgen Unutzer, M.D., M.P.H., an associate professor in residence in the department of psychiatry and behavioral sciences at the University of California at Los Angeles. Unutzer was the principal investigator on the study, which appeared in the September American Journal of Geriatric Psychiatry. The work was funded by the Health Care Financing Administration (now the Centers for Medicare and Medicaid Services) and the W.K. Kellogg Foundation.
The report is a secondary analysis of data collected over a seven-year period from nearly 2,600 Medicare participants aged 65 and older in the Seattle metropolitan area. The primary analysis of the data looked at the cost-effectiveness of preventive services for older enrollees in a Medicare+Choice plan.
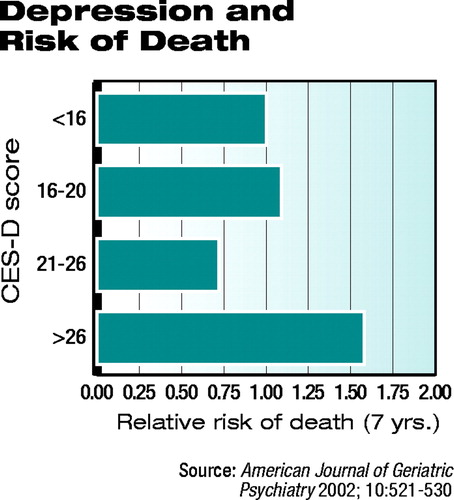
Unutzer and his colleagues wanted to study specifically the relationship between depression and mortality. The literature indicates a direct relationship—that is, any level of depression causes a statistically significant increase in the risk of mortality in elderly patients, Unutzer told Psychiatric News.
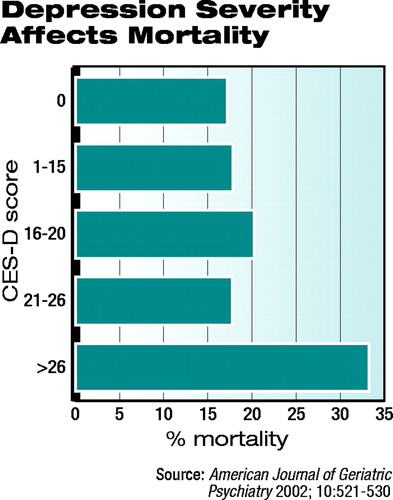 “We didn’t really find that in our study,” he said. “We found that there’s a very strong link if you have severe depression, with 30 percent of patients in the study who had severe depression dying over the seven-year course of the study, but only 15 percent of those with mild, moderate, or no depression dying by the end of the study.” Those figures are adjusted for demographic differences between the severe depression group and the whole cohort, health risk behaviors, and chronic medical disorders.
“We didn’t really find that in our study,” he said. “We found that there’s a very strong link if you have severe depression, with 30 percent of patients in the study who had severe depression dying over the seven-year course of the study, but only 15 percent of those with mild, moderate, or no depression dying by the end of the study.” Those figures are adjusted for demographic differences between the severe depression group and the whole cohort, health risk behaviors, and chronic medical disorders.
The twofold increase in the relative risk of death in patients with severe depression was comparable to the increase in the relative risk of death associated with other major health concerns common in the elderly, such as emphysema, heart disease, and cancer, and close to the increased risk associated with stroke or diabetes. However, they found no significant interaction between depression and other comorbid chronic medical disorders. Severe depression was linked to increased mortality rates in persons whose cause of death was cardiovascular disease.
 “It is not clear what accounts for this increase in mortality,” Unutzer and his colleagues wrote in the study report. “Proposed pathways include direct effects of depression on platelet functioning, autonomic regulation, cardiac conduction, or on the immune system or indirect effects of depression that are mediated through self-rated health or health behaviors.”
“It is not clear what accounts for this increase in mortality,” Unutzer and his colleagues wrote in the study report. “Proposed pathways include direct effects of depression on platelet functioning, autonomic regulation, cardiac conduction, or on the immune system or indirect effects of depression that are mediated through self-rated health or health behaviors.”
Understanding the link between risk of death and depression severity is critical, Unutzer said. “Health care professionals must take added steps to identify those patients and get them the treatment they need.”
The link was quite striking, Unutzer said. In the cost-effectiveness portion of the study previously published, Unutzer and his colleagues had found that persons with depression had roughly a 50 percent increase in their health care costs. Yet the increase was not accounted for by mental health care utilization.
“If the increased costs were a result of mental health care,” Unutzer speculated, “you’d say, OK, that makes sense—they are depressed, they are getting treatment, and that alone is increasing costs.”
The data revealed, however, that the increased costs were for medical treatment, not mental health care. In 1989, he said, the data showed that only around 10 percent of those identified with severe depression were getting any kind of mental health treatment. And only a handful, he said, had seen a psychiatrist.
“What that is telling us is that [psychiatrists] don’t see these patients, whether these elderly patients have severe depression or not,” Unutzer said. He believes the proportion of patients with severe depression being seen by psychiatrists has risen to somewhere between 40 percent and 50 percent, but the majority of their mental health care is done in the primary care, family practice, or internal medicine areas.
Progress is being made in some ways, however—there are newer, safer antidepressants, and more primary care doctors are willing to prescribe antidepressants. Nonetheless, “the majority of those prescriptions are one-time only with no refills and no follow-up. So there’s a huge gap in this age group between those needing treatment and those getting adequate basic treatment.
“We [as psychiatrists] need to think about what it is we can do to reach out not only to the patients but also to our colleagues in primary care.” There is still a huge gap, observed Unutzer, between the level of care given to seniors with depression by primary care doctors and that given by psychiatrists.
Unutzer is now studying whether the high mortality rates associated with severe depression in the elderly can be reduced through adequate and more appropriate treatments.
The study, “Depressive Symptoms and Mortality in a Prospective Study of 2,558 Older Adults,” is posted on the Web at http://ajgp.psychiatryonline.org/cgi/content/abstract/10/5/521. ▪
Am J Geriatr Psychiatry 2002 10 521



