Antipsychotic Comparison Finds Surprising Result
The first long-term, costeffectiveness study comparing olanzapine with a conventional antipsychotic drug produced surprising results.
Robert Rosenheck, M.D., told attendees at the Veterans Affairs (VA) Summit at APA's annual meeting in May that a study by the VA's Cooperative Study Group on the Cost- Effectiveness of Olanzapine found that when olanzapine was compared with haloperidol in a 12-month, double-blind, randomized controlled trial, there were no significant differences between the two in study retention; positive, negative, or total symptoms of schizophrenia; quality of life; or Parkinsonian extrapyramidal symptoms (EPS).
Rosenheck is director of the Veterans Administration Northeast Program Evaluation Center and a professor of psychiatry and public health at Yale School of Medicine.
Olanzapine was associated with reduced akathisia and with lower scores on measures of tardive dyskinesia in a secondary analysis including only observations during treatment with the blinded study drug. Small but statistically significant advantages were observed on measures of memory and motor function, but the drug was also associated with reports of weight gain.
Extra costs to the VA of using olanzapine instead of haloperidol ranged from $3,000 to $9,000 per patient per year, according to the study.
Olanzapine, which is the most widely used of the atypical antipsychotics, had worldwide sales of $3.7 billion in 2002.
The study group hypothesized that olanzapine would outperform haloperidol on three primary outcomes: demonstrating fewer symptoms, better quality of life, and lower costs to the VA. Costs to the VA, the group assumed, would be lower because the higher costs of olanzapine would be more than offset by lower costs of inpatient VA care.
The hypotheses relied on earlier studies that had found that olanzapine was associated with fewer EPS than haloperidol, greater improvement in symptoms and quality of life, and lower total health costs.
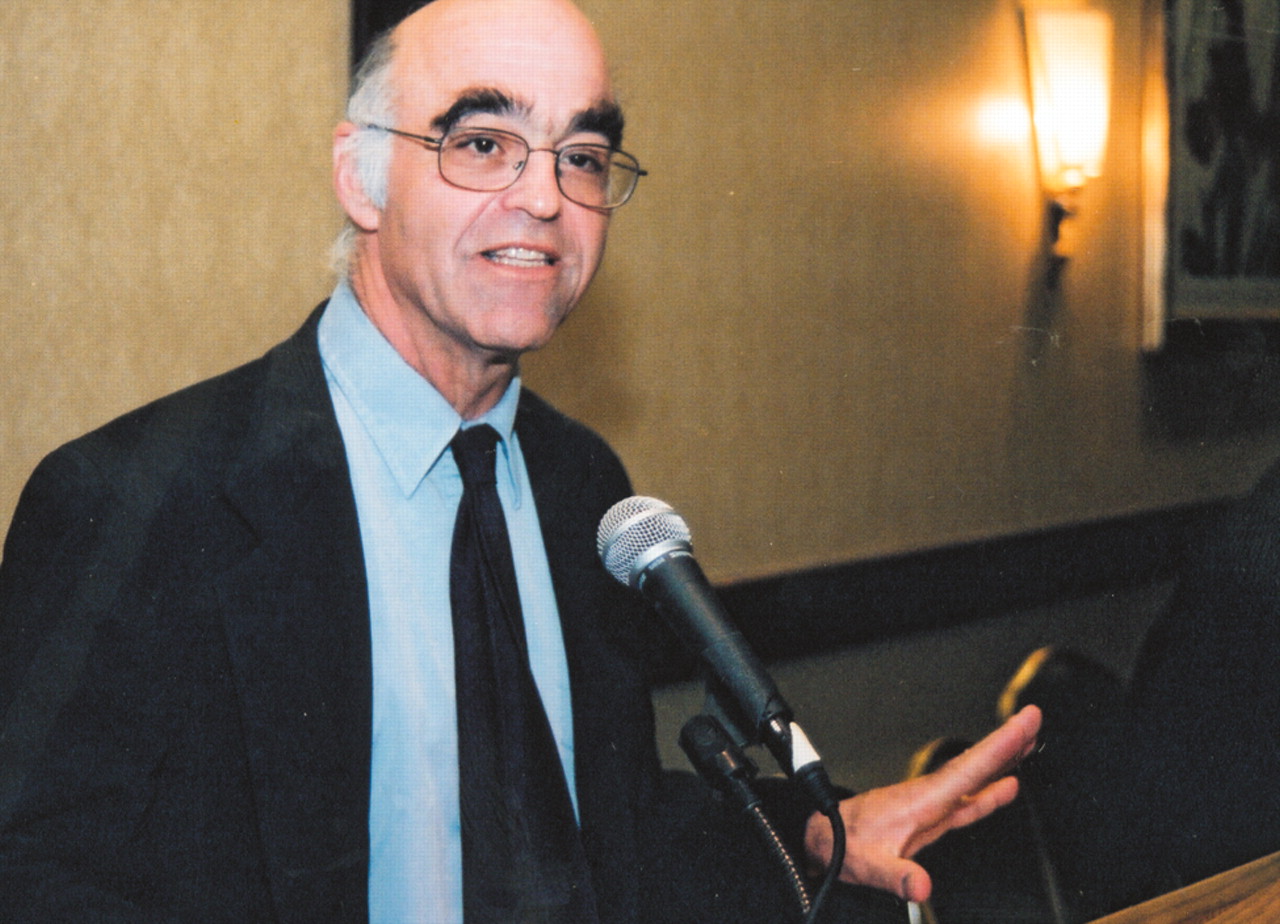
Robert Rosenheck, M.D.: "An important clue is that haloperidol patients did much better in terms of retention in the VA study. . . ."
Three hundred and nine VA patients diagnosed with schizophrenia or schizoaffective disorder were randomly assigned to flexibly dosed olanzapine (5 mg to 20 mg) or haloperidol (5 mg to 20 mg) and treated for 12 months at 17 VA medical centers.
There was no significant difference between the two groups in terms of the length of time members participated in the study, nor was there a significant difference in the proportion of patients in each group who completed the entire trial or in the reasons for discontinuation.
There were no significant differences between the groups on any measure of mental health service use or costs to the VA, exclusive of the cost of medication. Rosenheck suggested several possible reasons that the results of the VA study are less favorable to olanzapine than those reported in some previous trials.
"An important clue," he said, "is that haloperiodol patients did much better in terms of retention in the VA study than in other studies, while olanzapine patients in the VA study showed retention patterns that are similar to those of other studies."
In the International Collaborative Trial, one of Eli Lilly's FDA manufacturer's registration trials, 66.5 percent of patients receiving olanzapine completed six weeks of treatment, compared with 46.8 percent of patients receiving haloperidol.
In the VA study, in which haloperidol patients received prophylactic benztropine to prevent the development of EPS, 71 percent of the subjects completed six weeks of treatment, a slightly higher rate than for olanzapine (70 percent). Benztropine was available to patients receiving olanzapine if they developed EPS, but was not prescribed as a preventative measure. It was prescribed as a preventative measure for patients on haloperidol because of the likelihood that they would develop EPS without the medication, according to Rosenheck.
Studies producing results that are more favorable to olanzapine than to haloperidol, Rosenheck said, permitted use of benztropine only after the patient demonstrated a need for such medication. Such treatment protocols increased the risk of EPS and, more importantly, of akinesia without frank Parkinsonian symptoms. The presence of akinesia could be mistaken for a lack of response to the medication, according to Rosenheck.
In addition, the presence of EPS could introduce rating bias because the raters could surmise that the patient was receiving haloperidol.
Rosenheck also suggested that the use of an analytical technique that relies on the Last Observation Carried Forward (LOCF) method could have biased previous studies. In the LOCF, data collection ceases when a patient terminates the study drug, so the last assessment is the endpoint for comparison. LOCF can produce biased results when one group stays on a drug longer than the other for reasons that do not relate to the drug's efficacy.
The study was conducted under a contract between the VA Cooperative Studies Program and the Eli Lilly Corporation. It is under journal review. ▪



