Psychiatry Continues to Rebound, Match Results Show
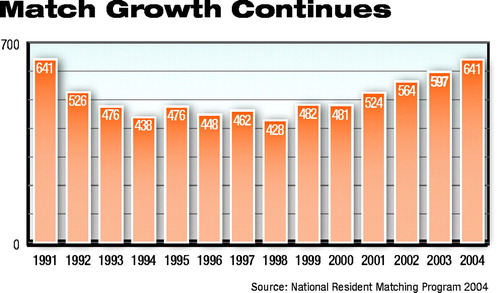 A total of 641 U.S. senior medical school graduates matched into general psychiatry residency programs around the country this year.
A total of 641 U.S. senior medical school graduates matched into general psychiatry residency programs around the country this year.
That figure is up from 597 in 2003, according to the National Residency Matching Program.
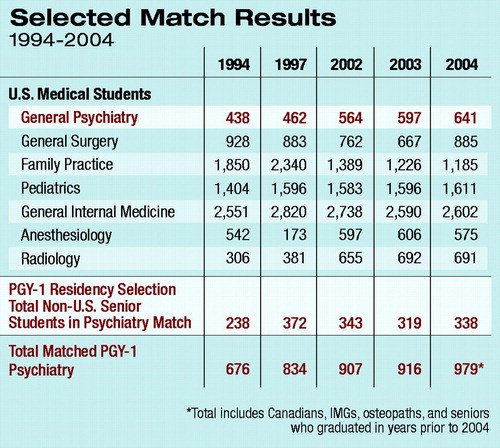 In addition, 338 students—including mostly international medical graduates (IMGs), Canadian students, and U.S. seniors who had graduated in previous years—also filled slots this year, for a total of 979 students entering PGY-1 general psychiatry residency positions this summer.
In addition, 338 students—including mostly international medical graduates (IMGs), Canadian students, and U.S. seniors who had graduated in previous years—also filled slots this year, for a total of 979 students entering PGY-1 general psychiatry residency positions this summer.
“I believe the exciting advances in neuroscience are in part responsible for this increase,” said Deborah Hales, M.D., director of APA's Division of Education and Career Development. “Research on the genetics of mental illness was named the number-two scientific ‘breakthrough of the year’ by Science magazine in its December l9, 2003, issue. In addition, the humanistic aspects of psychotherapy and the autonomy of psychiatric practice are other reasons we can hope to see this increase continue.”
An undetermined number of IMGs are also likely to enter psychiatry programs outside of the match to fill the remaining slots, said Area 4 Trustee Sydney Weissman, M.D., who has for years monitored match figures and workforce issues in psychiatry.
A small number of U.S. graduates entered double- and triple-board psychiatry programs this year: internal medicine/psychiatry (14); pediatrics/psychiatry/child psychiatry (18); and family medicine/psychiatry (9).
Weissman said the trend continues to be up for the profession. He noted, however, that the mental health needs of the American population far outstrip the psychiatric workforce, and that colleagues in primary care and other branches of medicine are likely to have to continue to pick up the slack.
“We have made significant progress in recruitment from 1998, when only 428 U.S. seniors selected PGY-1 general psychiatry residencies,” Weissman said. “We must remember that without the support of our medical colleagues, psychiatrists cannot deliver all of the medically informed mental health care in our country. We must assure that medical education for medical students and nonpsychiatric residents contains a critical core of psychiatric knowledge and training.”
The annual match is conducted by the National Resident Matching Program (NRMP), a private, not-for-profit organization established in 1952 to provide “an orderly and fair mechanism” to match the preferences of applicants to U.S. residency positions with the preferences of residency program directors for those applicants.
This year 25,246 applicants participated in the match, a 5.3 percent increase in participation since 2003. For the first time ever, more than 20,000 matches were made to first- and second-year residency positions, according to the Association of American Medical Colleges.
James Taylor, president of the NRMP, was quick to point to the increase in match participants as an indicator of the overall vitality and importance of the match, in light of a lawsuit filed by some medical students and residents claiming that the match process violates antitrust laws (Psychiatric News, June 7, 2002).
“The notable increase in applicants and residency positions this year indicates a high level of support and a continued confidence in the fairness of the match,” Taylor said. “It also once again demonstrates how important the match is to medical education and sends a clear message to those who want to dismantle the process.”
Data from each year’s match serve as an indicator of career interests among residency applicants and a prognostic indicator of the future physician workforce profile. Here are some highlights from this year’s match:
• U.S. medical school seniors filled 84.8 percent of the available first-year general surgery positions, up from 82.7 percent last year. This marks the second successive year of an increase in the surgery fill rate for U.S. seniors.
• 78.8 percent of PGY-1 family practice residency positions were filled, up 2.5 percentage points from last year. U.S. medical school seniors matched to 41.4 percent of those positions, a slight decrease from 2003. Family practice programs have experienced a steady decrease in the percentage of U.S. medical school seniors matching to their positions since 1996.
• Pathology programs continue to experience a higher percentage of positions filled through the match, a trend that began four years ago. This trend also holds true for U.S. medical school senior applicants to these programs; the percentage of PGY-1 pathology positions filled by U.S. medical school seniors has almost doubled since 2000 (to 61.2 percent in 2004).
Weissman said this year’s match figures generally reflect the continuing resurgence of specialty medicine after a period of decline in the 1990s.
A combination of scientific and career-lifestyle factors continues to drive the choices medical school graduates make, he observed.
“I believe there are two important variables,” Weissman said. “The first relates to the specific aspects of a medical discipline, its science, and how it is uniquely practiced. In psychiatry we have seen an explosion in the neurosciences and an invigoration and sharpening of our use of the psychotherapies.
“The second variable relates to the standing of the discipline in the eyes of medicine and our society, income patterns, and the impact of practice on lifestyles. I do not see many significant shifts in the near future in the broad area defined by this variable.” ▪



