Getting Fatal Illness Diagnosis May Lessen Suicidal Ideation
Contrary to popular belief, receiving a diagnosis of a fatal illness may not exacerbate the risk of suicide, but rather diminish it.
So suggests a large international study of individuals at high genetic risk of an incurable neurodegenerative illness—Huntington's disease.
The study was headed by Jane Paulsen, Ph.D., a professor of psychiatry and neurology at the University of Iowa. It involved researchers at 43 sites in five countries, all of whom received training to ensure interrater reliability of data collection for the 4,171 subjects.
Each subject was at high risk for Huntington's because it is an autosomal-dominant disease, and they had a parent with it.
Each subject was evaluated with the Unified Huntington's Disease Rating Scale. This is a standardized clinical rating scale that assesses persons on four components of Huntington's disease: motor features such as gait, postural stability, and jerky, involuntary movements; functional capacity; cognitive ability; and psychiatric symptoms, such as anxiety, depression, irritable behavior, delusions, hallucinations, and suicidal thoughts.
Motor-feature findings for the subjects then allowed them to be grouped into one of four neurological categories: normal, nonspecific motor abnormalities or soft signs of Huntington's, motor abnormalities indicating possible Huntington's, and unequivocal motor abnormalities indicating definite Huntington's.
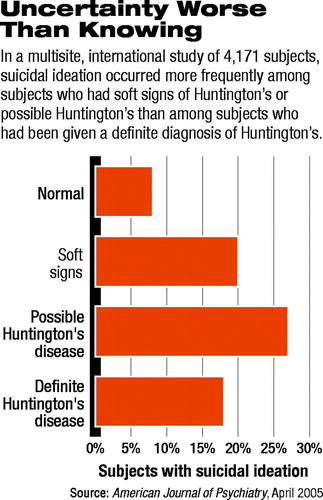
The researchers then compared the four groups on suicidal ideation. Suicidal ideation increased significantly from group two to group three, but then decreased significantly from group three to group four (see chart on page 32).
The scientists then focused only on those subjects who had received a definite diagnosis of Huntington's, divided them into five stages of illness, and looked to see whether subjects in one illness stage had more suicidal ideation than those in another illness stage. They found that illness stage did in fact make a difference.
There was a significant increase in suicidal ideation between stage one and stage two, a time when driving, managing finances, and other activities of daily living become increasingly constricted, and patients become increasingly dependent on others. But the proportion of individuals with suicidal ideas subsequently decreased with each stage beyond stage two.
These findings have several important implications, Paulsen and her team concluded in their report, which appeared in the April American Journal of Psychiatry. First, the greatest period for suicidal ideation in people at genetic risk of Huntington's appears to be when they start to have symptoms of the illness and fear that they might have it.
Second, once people know they have Huntington's, their greatest risk of suicidal ideation seems to be when their physical independence diminishes and they become increasingly dependent on others. Third, receiving a diagnosis of Huntington's appears to provoke less suicidal ideation than not knowing whether one has the disease.
This last finding, Paulsen and her coworkers said, contradicts the“ widely held belief among clinicians that being given a diagnosis of Huntington's disease (or other devastating diseases) will worsen depression, instill hopelessness, and increase suicidal ideation...[and] that delaying diagnosis of terminal, fatal, and/or devastating disease somehow protects the patient (albeit temporarily) from the trauma of the disease....[In fact] the opposite may be true.”
What's more, they suggested, “Perhaps the frequency of suicide [in this population] may be reduced by the expedient diagnosis of Huntington's disease combined with appropriate treatment of depression.”
Unfortunately, though, it is unknown exactly what role depression plays in suicidal risk among Huntington's patients and whether depression treatment reduces such risk. Also, studies that have attempted to determine the percentage of Huntington's patients who commit suicide have produced highly conflicting results—anywhere from seven to 200 times the rate in the general population.
Nonetheless, data do suggest that suicide rates among Huntington's patients are greater than those found among patients with other kinds of neurodegenerative or medical diseases. As Paulsen pointed out to Psychiatric News, “Depression is one of the primary symptoms of Huntington's disease and is highly treatable.”
The study was financed by the National Institutes of Health, Huntington's Disease Society of America, Huntington's Society of Canada, and Hereditary Disease Foundation.
The study, “Critical Periods of Suicide Risk in Huntington's Disease,” is posted online at<http://ajp.psychiatryonline.org/cgi/content/full/162/4/725>.▪
Am J Psychiatry 2005 162 725



