Caffeine, Alcohol Dependence May Share Genetic Traits
Caffeine dependence and alcohol dependence may share, at least to some extent, a common genetic vulnerability, a study reported in the December 2005 American Journal of Psychiatry suggests.
Forty-four newly pregnant women participated in the study. A diagnostic interview was conducted with each subject to determine caffeine dependence, alcohol abuse or dependence, or other psychiatric disorders. Caffeine dependence was defined by meeting DSM-IV criteria for lifetime substance dependence applied to caffeine use.
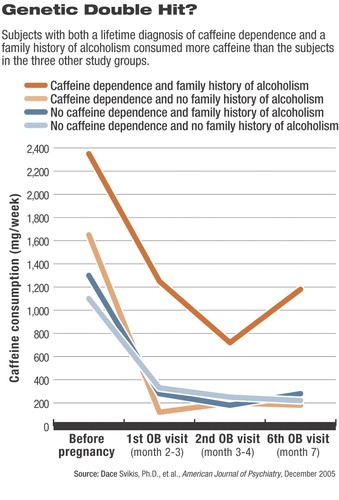
Of the 44 women, 10 had no caffeine dependence and no family history of alcoholism, nine had no caffeine dependence and a family history of alcoholism, 11 had caffeine dependence and no family history of alcoholism, and 14 had both caffeine dependence and a family history of alcoholism.
The subjects were instructed by their obstetrician to stop using caffeine during pregnancy since it has been linked with miscarriage and reduced fetal growth. The women were likewise assessed at three time points throughout pregnancy for caffeine consumption. Consumption was determined by both self-report and saliva samples.
The researchers then attempted to see whether subjects' caffeine consumption throughout their pregnancies was related to whether they were caffeine dependent, had a family history of alcoholism, or both.
Forty-three of the 44 subjects attempted to eliminate completely or cut back their caffeine use during pregnancy, and most made substantial strides in this direction. Nonetheless, at all time points, caffeine-dependent subjects consumed more caffeine than did those without such a dependence. Similarly, subjects with a family history of alcoholism consumed more caffeine than did those without such a history. And those with both a lifetime diagnosis of caffeine dependence and a family history of alcoholism consumed more caffeine than did the caffeine-dependent subjects, the subjects with a family history of alcoholism, and the subjects with neither caffeine dependence nor a family history of alcoholism (see chart).
In fact, even after a lifetime history of daily cigarette smoking, a lifetime history of alcohol abuse or dependence, or a lifetime history of any other psychiatric disorder was taken into consideration, subjects with caffeine dependence and a family history of alcoholism consumed between three and five times more caffeine than did the other subjects.
Thus, caffeine dependence and alcohol dependence may be genetically related, the researchers concluded in their study report.
“I was surprised by the strength of the relationship between a family history of alcoholism and the patterning of caffeine use in pregnancy,” Dace Svikis, Ph.D., a professor of psychology at Virginia Commonwealth University and lead investigator of the study, told Psychiatric News.
Still other results from the study suggest that caffeine dependence and alcohol dependence are genetically related to nicotine dependence as well. For instance, those subjects with both caffeine dependence and a family history of alcoholism were six times more likely to report a history of daily cigarette smoking than were subjects without both characteristics.
Finally, the study may shed some light on the prevalence of caffeine dependence in the general population. More than half of the subjects met criteria for lifetime substance dependence applied to caffeine use (25 subjects) and reported using caffeine to avoid withdrawal symptoms (23 subjects). According to the authors, the only previous study on the prevalence of caffeine dependence was a random-digit telephone survey conducted of 162 caffeine users in Vermont. In that study, 30 percent of subjects met the DSM-IV substance dependence criteria applied to caffeine.
These results have some practical implications, the investigators suggested. “[The] caffeine-dependence diagnosis may be a useful clinical and scientific marker for vulnerability to dependence on other drugs of abuse. Because there is little social stigma attached to caffeine use, self-reports may be more accurate for caffeine dependence than for problematic use of alcohol or drugs.”
Moreover, Svikis said, “When treating pregnant women, it is important to be cognizant of not only their use of alcohol, tobacco, and other drugs, but also caffeine. Women who are caffeine dependent and have a family history of alcoholism may need help in reducing or eliminating their use of caffeine.”
The study was funded by the National Institutes of Health.
“Caffeine Dependence in Combination With a Family History of Alcoholism as a Predictor of Continued Use of Caffeine During Pregnancy” is posted at<http://ajp.psychiatryonline.org/cgi/content/full/162/12/2344>.▪
Am J Psychiatry 2005 162 2344



