Afghans Build MH System With Only Two Psychiatrists
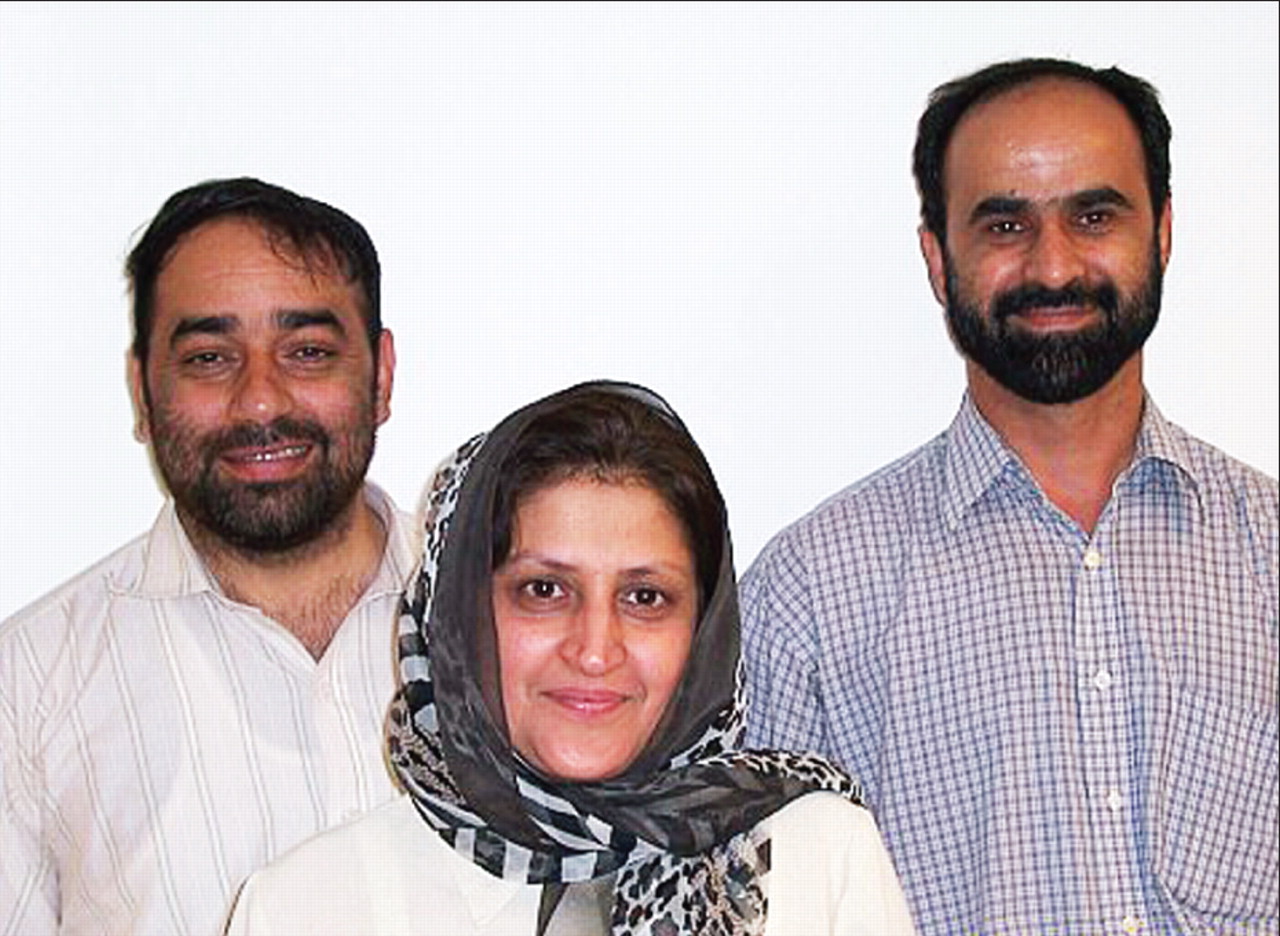
From left, Ruhullah Nassery, M.D., Alia Ibrahim Zai, M.D., and Hafizullah Faiz, M.D., visit Johns Hopkins and other U.S. medical institutions to learn about ways to improve mental health care in Afghanistan.
Credit: Anita Everett, M.D.
Three Afghan doctors toured U.S. medical schools and hospitals in early July as part of a long-term process to improve mental health services in Afghanistan.
Since the fall of the Taliban regime six years ago, the Afghan government has added mental health services to the basic package of health services available to its populace. Government officials placed mental health in the first tier of services, along with preventive medicine, children's health, disability services, and infectious diseases.
Warfare in the country has increased symptoms of depression and anxiety among many of the country's people but has also made it hard to build up the mental health system and train health care workers.
Afghanistan has only two fully qualified psychiatrists, and one works in the ministry of education, said Alia Ibrahim Zai, M.D., director of the National Mental Health Directorate of the Ministry of Public Health, during a meeting with psychiatrists, administrators, and others at the Johns Hopkins Bayview Medical Center in Baltimore.
Most care for the mentally ill in Afghanistan is provided by 40“ junior” psychiatrists— like Zai, general practitioners with some additional psychiatric training—or by 30 nurses who have received some psychiatry training. Throughout the country, there are five community-based inpatient centers, 11 outpatient mental health facilities, one day-treatment center, and a single, 60-bed tertiary care psychiatric hospital. The choice of psychiatric medications is limited to the World Health Organization's list of essential drugs.
Some care for the mentally ill has been provided by traditional healers who may, for example, chain their patients at shrines where ancient heroes are buried. Rather than ignore or fight these healers, the ministry has sought to forge relationships with them that have allowed physicians to visit patients twice a month to give antipsychotic drugs.
“We don't want to force change,” said Ruhullah Nassery, M.D., national mental health coordinator for the ministry. “The healers already have the faith of the people. We have long discussions with them about medications and substance abuse.”
The key to improving services will be better integrating mental health into primary care clinics, said Alia. To that end the ministry has given another 300 general practitioners more training in psychiatry.
The trip was part of an ongoing program by the Afghan and U.S. governments and some nongovernmental organizations (NGOs) to help develop and expand mental health services in Afghanistan. USAID, the World Bank, the European Commission, and the Substance Abuse and Mental Health Services Administration (SAMHSA) convened a planning conference in Kabul, Afghanistan's capital, in May 2006. Health policy in Afghanistan is determined by the government but financed and carried out by various international NGOs, said Winnie Mitchell, M.P.A., an international officer at SAMHSA.
Afghan doctors have met, either in person or by teleconference, with outside experts to discuss suicide prevention, reducing seclusion and restraint, and how to integrate primary and mental health care. Regular conference calls help cement these relationships and explore new questions as they arise, said Mitchell.
At present, about 20 percent of patients in the country's single psychiatric hospital are restrained, often with chains. The ministry has begun a “chain-free” initiative to eliminate them in the hospital and to follow patients at home after discharge to ensure appropriate controls that do not involve chains are available there.
The Afghan system has suffered not only from the aftereffects of the repressive and violent Taliban years, but also from the continuing instability and fighting in the country today, said Nassery. Many doctors and health workers have left the country, as they did during the Soviet occupation of Afghanistan in the 1980s. Even the ones who stay may have difficulties traveling to provincial cities to train health workers.
Nevertheless, the doctors have met people at Hopkins and other institutions who are interested in visiting Afghanistan to help train other health care professionals, said Nassery.
“We can see training working in both directions,” he said.“ In the short term, American or European psychiatrists and psychologists could come to Afghanistan to train people there. In the longer term, we could send some Afghan physicians to the U.S. for residencies, and they could return and set up similar programs in our country.”
Ultimately, their trip to the United States served as an important source of ideas for the Afghan physicians.
“The system here is long-established,” said Nassery. “We can adapt some of your programs for use in Afghanistan but probably not copy them exactly.” ▪



