Psychosocial Benefits Accrue When Psychotherapy Part of Treatment
Treatment consisting of a nine-month course of intensive psychotherapy and mood-stabilizing medication for patients with bipolar depression has been found to improve the patients' overall functioning, relationship functioning, and life satisfaction, according to a study published in the September American Journal of Psychiatry. These psychosocial benefits of intensive psychotherapy further support its use in the treatment of bipolar depression.
Patients in the study, conducted by David Miklowitz, Ph.D., and other researchers who participated in t he National Inst it ute of Mental Healt h's Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), had been diagnosed with bipolar I or bipolar II depression. They received treatment for acute depressive episodes when they were randomly assigned to undergo either 30 one-hour sessions of intensive psychotherapy over nine months or three one-hour sessions of collaborative-care educational counseling over six weeks.
Three types of psychotherapy were offered in the intervention group, depending on the study sites' expertise and the availability of patients' family members. Cognitive-behavioral therapy helped patients learn to change negative self-statements and dysfunctional beliefs. Interpersonal and social rhythm therapy emphasized the regularity of sleep/wake rhythms to maintain mood stability. Family-focused therapy sessions involved the patient and at least one family member, and effective communication and problem-solving skills were taught to both. In contrast, the collaborative care included providing the patients with a self-care workbook and an educational videotape about bipolar disorder and three one-hour sessions focused on implementing self-management tools and developing a relapse-prevention plan.
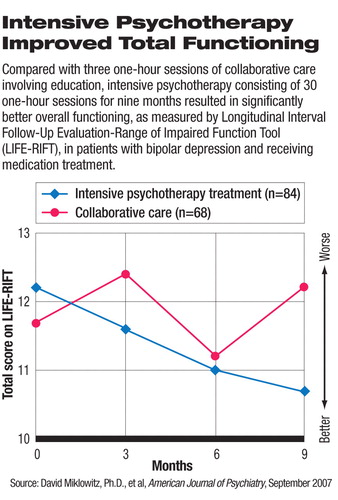
Of the 152 patients who participated in the study between September 1999 and July 2005 and had functioning assessment data available for analyses, 84 received intensive psychotherapy and 68 received collaborative care. Patients in the intensive psychotherapy group had statistically significantly better overall functioning as measured by the total score on the Longitudinal Interval Follow-Up Evaluation-Range of Impaired Functioning Tool (LIFE-RIFT) over the study period.
The intensive psychotherapy group also did better in the relationship functioning and satisfaction domains within the LIFE-RIFT, but there was no significant difference in the scores of work/role functioning and recreation domains between the intensive psychotherapy group and the collaborative care group.
The three types of psychotherapy appeared to be comparable in effectiveness in all measurements of functioning.
“Although the impact of intensive psychotherapy on functional improvement demonstrated modest effect sizes compared with collaborative care, given the significant functional impairment associated with bipolar disorder, even modest gains are clinically meaning,” Stephen M. Strakowski, M.D., wrote in an accompanying editorial.
In an article in the April Archives of General Psychiatry, the same authors reported the clinical outcomes of this STEP-BD study (Psychiatric News, May 4). Patients with bipolar depression receiving adjunctive intensive psychotherapy saw statistically significant improvement in terms of year-end recovery rates and shorter time to recovery compared with the patients in collaborative care. The social-functioning benefits documented in this study strengthened the role of intensive, long-term psychotherapy, rather than brief education, in the treatment plan.
The STEP-BD study involved 19 clinical centers and associated community partners across the country (see Original article: New Study Questions Common Bipolar Depression Treatment). A number of substudies were conducted within the overall program, which reflected “real-world” clinical practice for treatment of bipolar disorder and continue to generate clinical data for guiding optimal treatment approaches and future research directions.
“Intensive Psychosocial Intervention Enhances Functioning in Patients With Bipolar Depression: Results From a 9-Month Randomized Controlled Trial” is posted at<http://ajp.psychiatryonline.org/cgi/content/full/ajp;164/9/1340>. An abstract of “Psychosocial Treatments for Bipolar Depression” is posted at<http://archpsyc.ama-assn.org/cgi/content/abstract/64/4/419>.▪



