Funding, Logistics Deter Electronic-Record Adoption
Electronic medical records (EMRs) enhanced patient care and increased patient safety for the majority of health care professionals who responded to an annual survey of EMR use.
The annual survey of 819 health care physicians and other health care professionals by the Medical Records Institute (MRI)—a Boston-based group that advocates greater digital record use in health care—included two-thirds who identified themselves as having final or strong influence in EMR decision making. The MRI survey of 20 questions focused on areas such as strategic information technology priorities, factors driving adoption of EMRs, and major barriers to implementing EMR systems.
The most frequently cited barriers to EMR implementation were a lack of adequate funding or resources, anticipated difficulties in changing to an EMR system, and difficulty in creating a migration plan from paper to electronic documentation and recordkeeping.
Continued resistance to the use of EMRs by health care workers also was cited. Nearly one-third of respondents worked with an electronic record system that some colleagues refused to use.
For respondents who were able to get past those obstacles to EMR adoption, the technology appeared to have a large impact. More than two-thirds of respondents said the quality of care patients received had improved since adoption of EMRs in their organization. More than 90 percent also anticipated that the digital records would continue to improve the quality of care their patients receive over the coming 10 years.
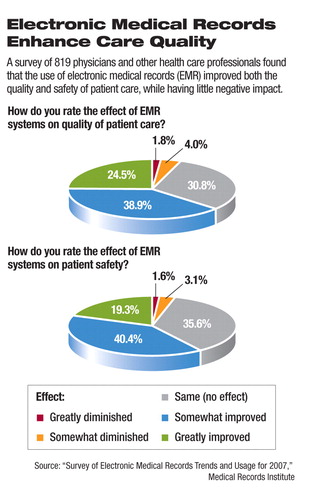
The safety impact also appeared significant. Three-quarters of respondents said patient safety was already improved by EMRs that their organizations have put in place. Again, more than 90 percent anticipated that EMRs would continue to improve patient safety over the next 10 years.
Further, the delivery of health care services has improved with the movement away from paper records. The majority of respondents reported that the efficiency of health care in their organization was improved by EMRs.
The adoption of health information technology by health care professionals is being driven by the need to improve clinical processes and work flow efficiency, according to the survey. The leading drivers for hospital use of EMR systems are a desire to improve patient safety, increase efficiency and convenience, and obtain the satisfaction of their physicians and“ clinician employees.” Medical practices are driven to adopt EMRs by a desire to improve patient-care documentation, improve efficiency and convenience for physicians, and allow remote access to patient information.
The most-used EMR “data capture” applications were those that tracked patient demographics, allergies and adverse reactions, and laboratory results. The least-used applications included pre-visit health-screening features and post-visit patient-education components.
The findings of this survey reflected conclusions reached by other research on clinicians' use of emerging digital record-keeping technology, according to Joy Grossman, Ph.D., senior researcher for the Center for Studying Health System Change (HSC).
A national study by the HSC reported in September that practice setting and size were the strongest predictors of the availability of clinical information technology to physicians. However, different types of clinicians had significant variation in their information technology adoption (Psychiatric News, October 19).
“The survey was fairly consistent with studies we have done on the functionality that is valued by physicians,” Grossman said, about EMRs' ability to track drug interactions.
Her research has indicated t hat increased convenience is a major factor driving more physicians to use EMRs. The survey-identified barriers to adoption—cost, anticipated difficulties in switching, and migration-plan challenges—also reflect what previous research has found.
The survey revealed another factor pushing more physicians to adopt EMRs—the anticipation of the Centers for Medicare and Medicaid Services' (CMS) moving toward pay-for-performance systems, Grossman told Psychiatric News (see Original article: CMS Physician Quality Reporting Initiative: Changes for 2008).
In the survey analysis, physicians with access to information technology for all five clinical activities were considered to have an EMR.
The ninth annual MRI survey also affirmed trends from previous years, including an increased use over the prior year of EMRs for e-prescribing in hospital settings, where its use by nurses and other staff continues to exceed physician use. Use of the Continuity of Care Record, which is a standard patient health summary that can be sent between health care providers, also has increased since 2006.
Despite the challenges of adopting EMRs, few reported abandoning the effort. Less than one-fifth of respondents reported deinstallation of one EMR system to replace it with another, and less than one-tenth reported deinstallation to revert to paper records.
Information from MRI's 2007 Survey of Electronic Medical Record Trends and Usage is posted at<www.medrecinst.com/MRI/emrsurvey.html>.▪



