Match Shows Slight Increase in Graduates Going Into Psychiatry
A total of 1,013 medical graduates will enter first-year psychiatry residency programs this year, a small increase over the previous year's total of 1,000.
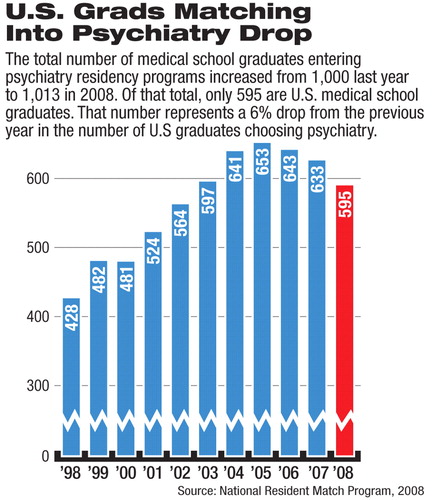
But the number of graduates from U.S. medical schools choosing psychiatry has dropped slowly but steadily for several years; this year's number—595—represents a drop of 6 percent from last year and 8.8 percent from 2005 (see chart).
These figures are part of the results released by the National Resident Match Program (NRMP), which conducts the annual “match” in which medical school graduates are matched with a residency program.
The match is looked at as a barometer of the future shape of medical practice. One notable trend in specialty choice this year was an increased interest in family medicine residency positions; 1,156 (or 7.6 percent) of U.S. medical school seniors matched to one of those positions, up from 7.2 percent last year.
The 2008 match results also indicate that plastic surgery, orthopedic surgery, dermatology, otolaryngology, diagnostic radiology, radiation oncology, and general surgery continued to be popular and competitive specialties. The number of students choosing anesthesiology increased from 448 in 2007 to 524 this year, while the number choosing general surgery increased from 826 to 888.
Psychiatry continues to rely on international medical graduates to fill many of its residency training slots. This year a total of 1,069 positions were offered, with 94.8 percent of those being filled.
U.S. medical school graduates accounted for 55.7 percent of the filled positions.
APA Trustee Sidney Weissman, M.D., a past president of the American Association of Directors of Psychiatric Residency Training who has maintained a long-time interest in workforce issues, told Psychiatric News that many of the factors affecting the choices and preferences of graduates are cultural and socioeconomic factors beyond the control of psychiatric educators.
But in an analysis of the match that Weissman sends each year to training directors and other interested parties, he suggested that there are steps that can be taken to recruit more graduates to psychiatry.
“Academic psychiatrists can place themselves when possible on medical school admission committees, ensuring that students with appropriate abilities to be physicians but who also have the capacity to potentially become psychiatrists are admitted to medical school and are subsequently enrolled.
“This will ensure in each medical school a pool of potential psychiatrists,” he said.
He also emphasized that the quality of the clerkship year is essential.
“For some students, the decision to become a psychiatrist is made prior to medical school, and the clerkship experience simply reinforces the decision,” he said. “For others, the clerkship experience coupled with other medical school experience is where they decide to become psychiatrists. With the development of new clerkship sites with the expansion of medical schools, we must be sure that they, as well as present sites, all offer outstanding training.”
The match, conducted annually by the NRMP, uses a computer algorithm to align the preferences of applicants with the preferences of residency program directors to fill the thousands of training positions available at U.S. teaching hospitals each year.
The NRMP is a private, not-for-profit organization established in 1952 to provide an orderly and fair mechanism for matching residents with residency programs.
The NRMP is sponsored by the American Board of Medical Specialties, American Medical Association, Association of American Medical Colleges, American Hospital Association, and Council of Medical Specialty Societies.
This year's match results are posted at<www.nrmp.org>.▪



