Innovative Funding Strategy Pays Off in California
Abstract
A drop in the number of patients treated after suffering a psychiatric crisis since passage of California's 2004 voter initiative to fund expansion of the state's public mental health system suggests that the system's treatment and prevention programs have been effective, according to new research.
California's Mental Health Services Act (MHSA), which established an annual tax on people who make over a million dollars a year and dedicated that revenue to public mental health programs, had distributed about $3.2 billion by Fiscal 2008-2009. That surge in funding appears to have helped expand noninstitutional community-based programs that provide management of serious mental illness and reduced the need for inpatient psychiatric care of people whose conditions have deteriorated due to lack of treatment, according to a study in the October Psychiatric Services.
The study, led by Tim Bruckner, Ph.D., an assistant professor in the Public Health Department of the School of Social Ecology at the University of California, Irvine, was based on previous research that used the incidence of involuntary treatment as a gauge of the overall functioning of public mental health systems.
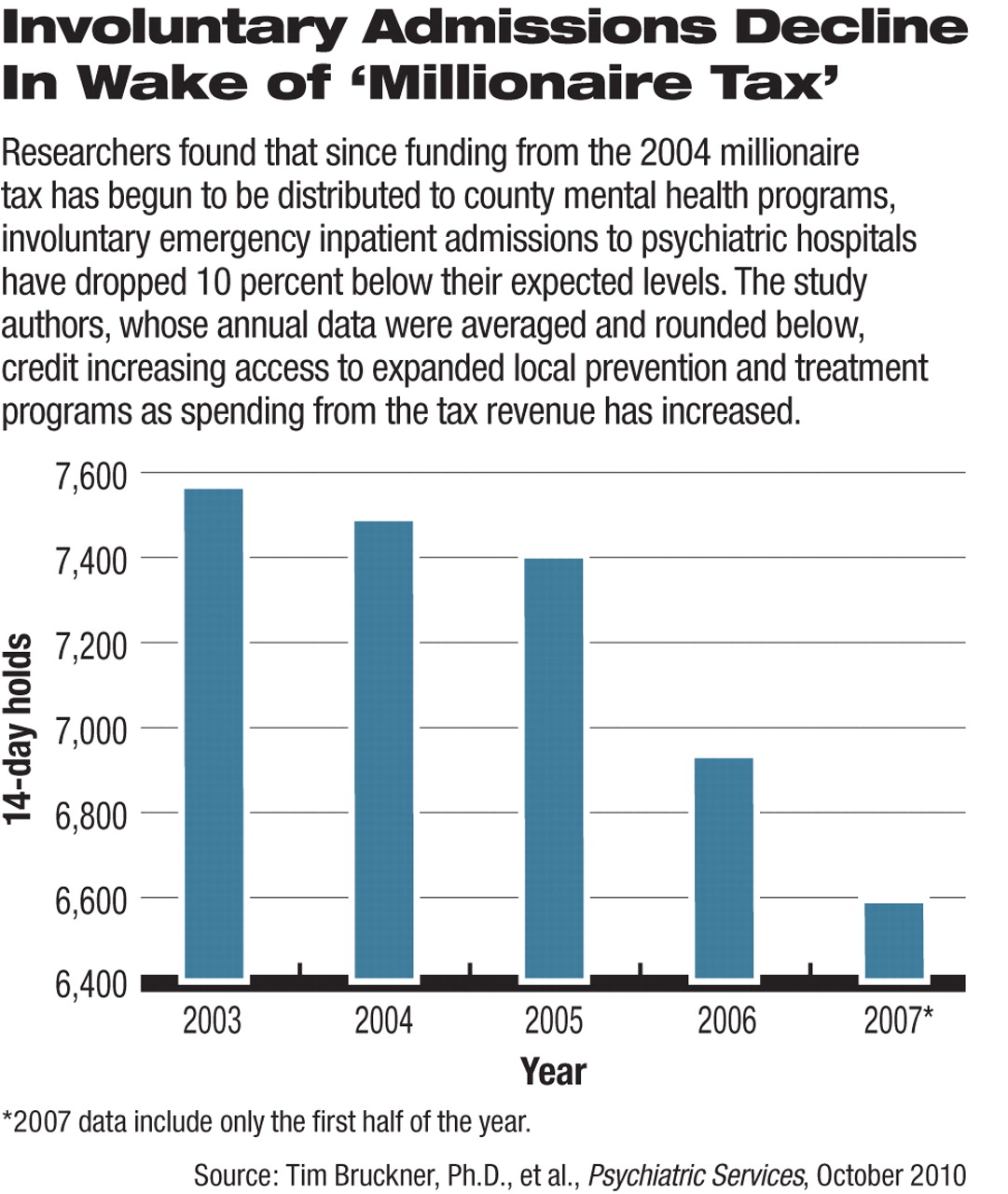
Based on this “canary in the coal mine” approach to assessing the effectiveness of the MHSA, Bruckner and colleagues examined the incidence of 72-hour and 14-day involuntary psychiatric civil commitments and found that the 14-day holds were 10 percent fewer by 2007, three years after the law took effect. The number of 72-hour holds did not fall below expected numbers after disbursement of MHSA funds, however.
The authors concluded that the lower-than-expected number of involuntary 14-day hospitalizations may indicate an important shift toward community-based treatment programs.
“Results indicate that the structure and funding of the MHSA may have provided enhanced resources and diverted clients to less-restrictive treatment settings,” Bruckner and his colleagues said.
Psychiatrists Seeing Positive Effect
It's an impact of the law that psychiatrists in the state also say they see.
Robert Cabaj, M.D., medical director of Community Behavioral Health Services in San Francisco's Department of Public Health and chair of APA's Council on Advocacy and Government Relations, told Psychiatric News that he agreed that the reduction in two-week emergency hospitalizations may be due to increased availability of community-based services funded by the 2004 law—especially intensive case management.
“I truly believe the added intensive case management in the counties (San Francisco, for example, was able to add more than 400 new intensive case management slots in the effort to ‘do what ever is needed’) has led to the reduced hospitalizations,” Cabaj said. “We have cut our acute inpatient psych beds in San Francisco by more than half, but have had no increase in recidivism or emergency services—an effect I explain solely by the increased access to care and intensive case management.”
Roderick Shaner, M.D., medical director of the Los Angeles County Department of Mental Health, told Psychiatric News that although followup data are required to assess whether the decrease in longer involuntary hospitalization found in the study will be reflected in better mental health outcomes, the study's findings reflect his anecdotal experiences.
“The great majority of California mental health system stakeholders believe that MHSA has had significant positive effects on many aspects of mental health treatment in California,” Shaner said. “Most remarkable among these positive effects is a more focused and effective approach toward community reintegration and improved quality of life for individuals with mental illness.”
Program Improvements Needed
Shaner noted that questions remain over how to improve the overall effectiveness of the range of programs and planning processes associated with the MHSA, including greater effectiveness for individuals with emergency mental health needs. The need to improve those programs is suggested by the study's finding that there was no decrease in 72-hour emergency hospitalizations.
Among those local programs are new prevention initiatives by counties, including the Early Psychosis Project, which Los Angeles County launched to identify people who are at risk for psychosis due to “destabilized lives.” The aim of the project is to prevent or minimize problems, Cabaj noted.
Another looming challenge that could undermine expansions in such local mental illness prevention and treatment efforts is a state budget shortfall of nearly $20 billion. In light of that budget gap, a growing number of legislators have raised the possibility of diverting some MHSA funds to other health programs not related to mental health.
“One argument in support of sustaining MHSA funds would involve demonstrated effectiveness of the counties' improved management and treatment of persons with severe mental illness,” noted Bruckner and colleagues.
Supporters of the MHSA funding program have emphasized that it should remain focused on local prevention and treatment programs since they offer far less expensive treatment than do inpatient facilities for patients who lacked such early interventions and have decompensated due to their untreated illnesses.
“Involuntary Civil Commitments After the Implementation of California's Mental Health Services Act” is posted at <http://psychservices.psychiatryonline.org/>.



