Data Show Reason for Concern if Mothers Carry Herpes Virus
Abstract
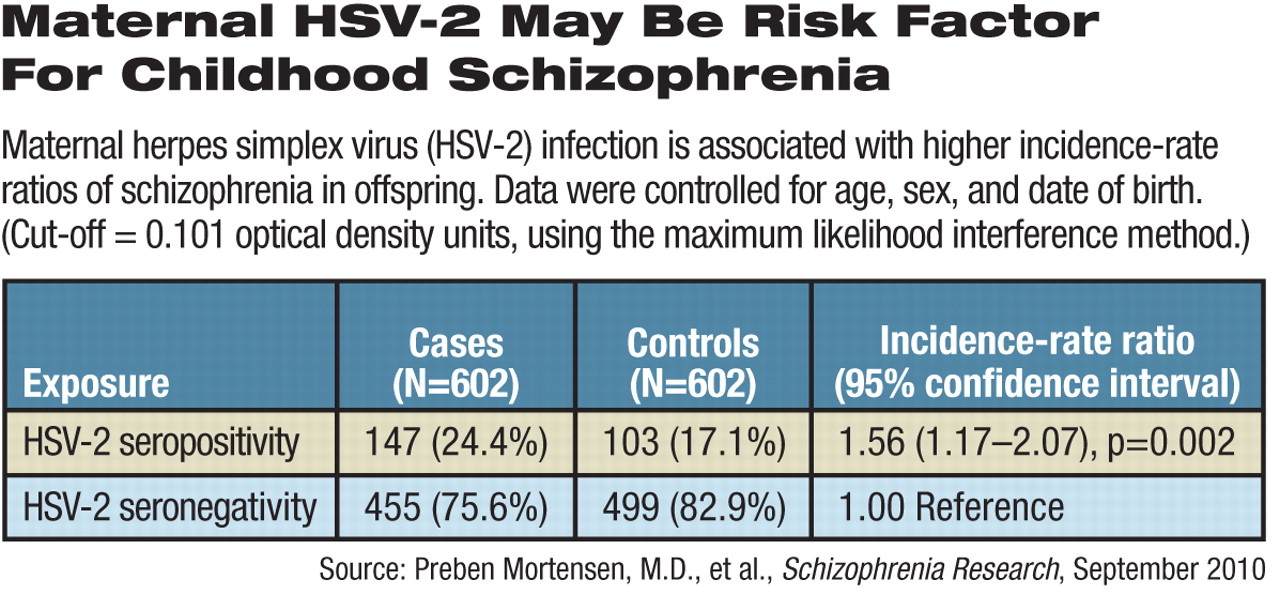
A large case-control study based on Danish birth and psychiatric records has added more evidence to back the theory that an association exists between mothers' infection with herpes simplex virus 2 (HSV-2) and the risk of schizophrenia in their children.
The results were unaffected by adjustment for place of birth, parental age, or immigrant status, wrote Preben Mortensen, M.D., and colleagues in the September Schizophrenia Research. Mortensen is a professor and director of the National Centre for Register-Based Research at the University of Aarhus in Denmark.
The study confirms a similar association published in 2008 by Stephen Buka, M.D., and others, but there have been several other reports on this potential relationship that have produced equivocal results. The prior studies were limited by small sample sizes, limited statistical power, and lack of data on some confounders, Mortensen noted.
The new research is based on 602 cases of schizophrenia among 1.5 million children born in Denmark from 1981 to 1994 and an equal number of controls matched for gender and exact date of birth. None of the controls had a history of schizophrenia at the time the evaluation was conducted.
Blood was drawn from newborns within a week of birth, but the antibodies reflected the mothers' exposure to infection, said the authors. “Maternal [immunoglobin G] is transferred across the placenta, and the child has not produced any specific amount of IgG at the age when the blood sample was taken.”
About 24 percent of the blood samples from schizophrenia cases had HSV-2 antibodies above the cutoff levels for seropositivity, compared with 17 percent of the samples from the matched controls, an incidence-rate ratio of 1.56.
Parental age, parents' immigrant status, maternal mental illness history, and whether the child was born in an urban area had no effect on the association between HSV-2 antibodies and schizophrenia.
The researchers did, however, note a trend toward greater schizophrenia risk among children born before 36 weeks of gestation, but absolute numbers were so small (seven cases and two controls) that gestational age had no statistically significant effect on the association.
The study was supported by a grant from the Stanley Medical Research Institute.
A second study, published in the September Archives of General Psychiatry by Danish, British, and American researchers (including Mortensen) and based on Danish and Swedish birth cohorts, suggested that as birth weight declined, risk for any psychiatric diagnosis increased. A similar pattern held true regarding schizophrenia for birth weights below 3,000 grams.
In Mortensen and colleagues' study of HSV-2 exposure, adjusting for parental history of mental illness reduced that ratio somewhat, but the effect was largely due to the father's mental illness history, said the authors. Of the 147 seropositive cases in that study, 34 fathers were diagnosed with mental illness, but 23 had diagnoses outside of the schizophrenia spectrum.
“If the association was due only to genetic stratification, it should be equally confounded by maternal mental illness,” they wrote.
However, there may be a path other than genetics through which the mothers contributed to schizophrenia risk, the researchers suggested. Risk for HSV-2 seropositivity is increased by early initiation of sexual activity, having more sexual partners, low socioeconomic status, and a history of other sexually transmitted diseases.
An abstract of “A Danish National Birth Cohort Study of Maternal HSV-2 Antibodies as a Risk Factor for Schizophrenia in Their Offspring” is posted at <www.schres-journal.com/article/S0920-9964(10)01365-4/abstract>. An abstract of “Birth Weight, Schizophrenia, and Adult Mental Disorder: Is Risk Confined to the Smallest Babies” is posted at <http://archpsyc.ama-assn.org/cgi/content/abstract/67/9/923>.



