Psychiatrists Overcame Challenges in Responding to Hurricane
Abstract
Wind. Rain. Flood. Fire. Darkness. Cold. Hurricane Sandy left an apocalyptic aftermath for residents of New Jersey and New York.
The storm flooded subways and highway tunnels, knocked out power around the region, destroyed beachfront communities, and left others in flames, under water, or uninhabitable. Gasoline was rationed. Weeks after the storm, city and state officials were still trying to get the lights on and find housing for tens of thousands of people.

Emergency personnel and equipment were marshaled in the lobby of Bellevue Hospital to help with patient evacuation after Hurricane Sandy struck New York at the end of October.
However, lessons learned from the two paradigm American disasters of the 21st century, September 11, 2001, and Hurricane Katrina, helped emergency-management agencies and health departments respond more effectively this time, said Sandro Galea, M.D., Dr.P.H., a professor and chair of the Department of Epidemiology at the Mailman School of Public Health at Columbia University.
“There’s a lot more awareness of the reality of mental health in the aftermath of trauma,” said Galea. “There is also a greater recognition of the importance of restoring basic services and their role in returning function to survivors as an essential health option.”
Hurricane Sandy left New Jersey psychiatrists struggling to connect with patients right after the storm, said Charles Ciolino, M.D., of Basking Ridge, N.J., chair of the New Jersey Psychiatric Association’s Disaster Preparedness Committee, in an interview with Psychiatric News. Downed trees and power lines made simply moving around difficult. (A tree crashed into Ciolino’s home during the storm.)
On the third day after the storm, he reached the general hospital where he has privileges and saw patients, who were variously experiencing exacerbation of anxiety disorders, addiction relapse, problems coping with storm-related physical injuries, and difficulty obtaining psychotropic medications because many pharmacies were closed because of lack of power, he said.
“Area psychiatrists helped in local emergency rooms and volunteered through the Red Cross for mental health response to shelters,” said Ciolino. “One of our retired psychiatrists, Dr. Margaret Thompsett, a cofounder of our Disaster Preparedness Committee, traveled from Massachusetts as a Red Cross national volunteer.”
Life is now gradually returning to normal for most people, he said. “But for some, especially those displaced from their homes and those with storm-related exacerbation of mental disorders, coping with ’a new normal’ will indeed be challenging.”
Devastated as residents were, the real mental health consequences of the storm will only arrive weeks or months from now.
“This is just the first stage,” said Ciolino. “There will be a long period of rebuilding physically and psychologically, so our psychiatrists will remain available to assist the Red Cross, social services, and mental health programs, in our efforts to help these people progress forward.”
Glenn Kashurba, M.D., of Somerset, Pa., was deployed to New Jersey within days of the storm as part of a Disaster Medical Assistance Team (DMAT). He performed general medical work and consulted on psychiatric issues—such as the status of evacuees in a shelter that housed indigent and chronically mentally ill individuals.
“The big problem they face when displaced is they don’t have their medications, and you have to quickly transition them to whatever the DMAT has in stock,” Kashurba said. Those changes can mean moving from the newer class of antipsychotics to older drugs or using benzodiazepines to tide patients over for a few days until they can reconnect with pharmacies.
Hospitals Forced to Evacuate
In New York City, lower Manhattan was first flooded and then lost power below 34th Street. The Veterans Affairs Hospital on 23rd Street was evacuated on Sunday as the storm roared in.
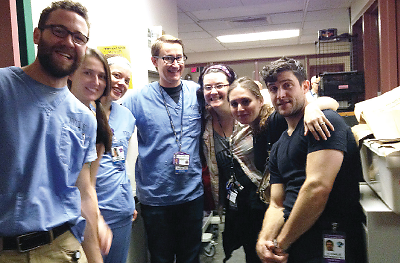
New York University psychiatry residents stayed at Bellevue Hospital during and after Hurricane Sandy to care for patients and help with evacuation. From left: David Stiffler, M.D. (PGY-3), Abigail Hawkins, M.D. (PGY-2), Kelly Kleinert, M.D. (PGY-2), Chris Racine, M.D. (PGY-4 and chief resident), Lori Bennett-Penn, M.D. (PGY-2), Jessica Eisenberg, M.D. (PGY-2), and Charlie Wittenberg, M.D. (PGY-2).
“On Monday, a huge flood poured into the ground floor of New York University’s Tisch Hospital, prompting its evacuation,” recalled former APA President Carol Bernstein, M.D., an associate professor of psychiatry, director of psychiatry residency training, and vice chair for education at NYU. “Then Bellevue Hospital lost power but the generators worked, until the fuel pumps in its basement got flooded.”
After that, first staff and then National Guard troops had to haul fuel up to the generators.
The Bellevue psychiatry department’s residents came in on foot and bicycle to help out, she said in an interview. “They were heroic,” she said. “Their commitment and selfless dedication were what you really know medicine is all about. I couldn’t have been more proud of them.” (see A Day One Resident Won't Forget).
On Wednesday evening, Bellevue received its official evacuation orders, although some patients had already been moved out, said Bernstein.
“About 150 psychiatric patients out of 300 were still left, including forensic patients,” she said. “The Bellevue staff worked furiously to find beds elsewhere to place them, mostly with other New York City Health and Hospital Commission hospitals.”
Group Homes Rendered Uninhabitable
Elsewhere in the city, one of the worst tragedies was the conflagration that consumed about 100 houses in the beachside Breezy Point and Belle Harbor sections of the Rockaway peninsula in Queens.
Nearby, 40 to 50 group homes for chronic psychiatric patients had to be evacuated in the Rockaways area because of flooding and power outages, said Seeth Vivek, M.D., chair of psychiatry at Jamaica Hospital Medical Center in Queens and vice president of the New York State Psychiatric Association.
“They all were moved to two local colleges,” Vivek told Psychiatric News. “Most were stable, but others had to go to emergency rooms. Many had lost their medications, and many pharmacies lost power and so could not fill prescriptions.”
Jamaica Hospital sent two mobile vans out each day, one to the Howard Beach area and one to the Rockaways, said Vivek. “Each van has supplies, plus one primary care physician and one psychiatrist along with support staff.”
New York City’s Department of Health and Mental Hygiene asked for volunteer psychiatrists to help staff a number of New York City Restoration Centers in the Bronx, Brooklyn, Staten Island, and Queens.
Disaster Psychiatry Outreach (DPO), a nonprofit organization founded in 1998, worked with the city health department and also put out a call for volunteer psychiatrists to help with the mental health response.
DPO holds training sessions when there are no disasters in progress—it staged one at last year’s APA annual meeting in May—but also trains new volunteers immediately after disasters in sessions lasting four hours to two days.
“Here in New York, the role for psychiatrists is still limited,” said DPO President Sander Koyfman, M.D. “Meeting basic needs comes first. Once the acute phase is over, we will provide services at some of the disaster assistance centers.”
Times have changed since September 11, Koyfman explained. “The current response is heartening,” he said. “Not only is mental health on the radar, but it is in the forefront of conversations.”
That sentiment was echoed by the chair of APA’s Committee on Psychiatric Dimensions of Disasters. “It’s impressive to hear from community leaders and politicians the language of disaster response,” said Robert Ursano, M.D., chair of psychiatry and director of the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences in Bethesda, Md. “There will be some PTSD in the hardest-hit populations, but there is likely to be even more chronic depression, substance use, and sleep problems—the most common aftermath of September 11.” 
More information about New York University’s psychiatry residents’ response to Hurricane Sandy is posted at http://psych.med.nyu.edu/education/residency-training/hurricane-response-efforts.
A Day One Resident Won't Forget
Marc Manseau, M.D., M.P.H., a fourth-year resident in psychiatry at New York University’s School of Medicine, recorded his own experiences during and after Hurricane Sandy:
…. Next, I learned that Bellevue was running on backup generators and had begun a partial evacuation. So, when I received an e-mail from a chief resident on Tuesday morning asking residents to come in and help, I barely had time to brush my teeth.
The hallways were dark and quiet when I arrived. The smell of generator diesel hung pungently in the air. Strangely, with the emergency room closed and none of the usual hospital work getting done, it was less busy than any routine shift….
The residents waited for instructions to carry out needed nonclinical tasks, from escorting discharged patients safely down 20 flights of stairs to walking medications or food up from the ground floor.
That might have infuriated us on a normal day, but we were able to take it in stride. Our Bellevue training had prepared us to work under the most difficult conditions, as long as we knew that we were doing our best for our patients….
As Tuesday turned into Wednesday (many of us lost track), conditions became both worse and more eerie. I walked past a darkened, empty ICU with many machines still beeping crazily, as the National Guard carried extremely ill patients down many flights in stretchers. The official evacuation was ordered on Wednesday afternoon, and we had to get everyone transferred by Thursday at noon.
The more psychotic patients peppered us with questions about why they weren’t being discharged or where the belt that they came into the hospital with was, and so on. It was fun watching my co-residents redirect these patients using their unique clinical styles in between filling out legal documents and transfer forms. Finally, the National Guard showed up to evacuate the unit just as we signed the very last piece of paperwork ….
Complex impressions and lessons of those days now swirl through my mind. I have come to respect my supervisors and colleagues more than I could ever imagine. I am also reminded once again of the vital importance and value of rigorous, intensive clinical training that prepares you for anything in clinical work and, to a certain extent, in life.



