CBT Addresses Most-Debilitating Symptoms in Chronic Schizophrenia
Abstract
Patients are taught to view challenges such as difficulty in information processing, psychiatric symptoms, and isolation as solvable problems that can be neutralized as they move toward their goals.
Recovery-oriented cognitive therapy (CT-R) appears to be highly successful in the treatment of individuals with chronic schizophrenia who have difficulty integrating into the community.
A new cognitive-behavior therapeutic strategy is helping patients overcome major obstacles to their recovery, especially the negative symptoms—lack of motivation, anhedonia, and asocial behavior—that are considered to be the most intransigent and disabling for patients with schizophrenia. The strategy has been implemented throughout the Philadelphia public mental health system and in Georgia (Psychiatric News, December 5, 2013).
In an interview with Psychiatric News, Paul Grant, Ph.D., a research assistant at the Aaron T. Beck Psychopathology Research Center in the Perelman School of Medicine at the University of Pennsylvania, discussed how CT-R is used in treating individuals with schizophrenia who are struggling with negative symptoms and other obstacles to recovery.
He said the strategy is based on research by him and colleagues showing that early emerging neurocognitive deficits lead to disappointing outcomes, which, in turn, cause individuals to develop defeatist beliefs; these beliefs engender what appear as negative symptoms. Through an often slow, laborious process, these beliefs can be addressed and corrected, allowing patients to achieve self-defined goals.
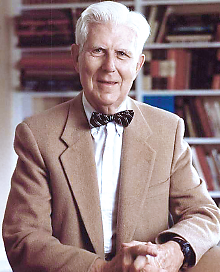
Aaron Beck, M.D.: Modified CBT for schizophrenia patients was found to improve their functioning and standard of living.
“Recovery started as a political movement and has become the aim and standard of care in the United States,” Grant said. “Most providers think that recovery is what they should be promoting, but they frequently do not know how to do so. Much of the work in this area by psychologists, psychiatrists, and others has been to counter stigma and show that recovery is possible and more common than many expect.
“Our program operationalizes each individual’s unique recovery path,” Grant said. “This is done by procedures that allow for establishing patients’ specific, motivating long-term goals—to form friendships, get married, to have children, to work. These valued goals are then broken down into manageable steps so that the individual can see that each successful step is getting him or her closer to the valued goal. Then, we help the individual begin positive action steps toward the long-term goal and identify obstacles that we help him or her remove.”
Such obstacles may include low energy, hallucinations, delusional beliefs, anger, or substance use and have psychological meanings that engender the defeatist beliefs associated with negative symptoms—for example, “I’m defective,” “I’m incapable,” “I don’t fit in.”
“We use the cognitive model to develop a formulation that is tailored to each person and helps to understand each obstacle,” Grant explained. “The formulation helps us develop a strategy to remove each obstacle to the person successfully achieving his or her personal goals.”
In a report in Psychological Services, Paul Grant, Ph.D., and colleagues describe the successful use of recovery-oriented CBT in the treatment of negative symptoms in a patient with schizophrenia. They describe “Mary,” a 57-year-old woman who lived at home with her sister and received help with most of her daily living activities. She spent the better part of each day alone. She had significant tardive dyskinesia caused by a long history of taking antipsychotic medications and experienced auditory and visual hallucinations on a daily basis. She believed that people were coming to kill her and that she needed to save local hospitals. Accordingly, she incessantly called the police department, the Federal Bureau of Investigation, local hospitals, and family members. This pattern of making phone calls occurred approximately 15 times a day prior to participating in treatment.
Treatment entailed 70 individual 50-minute sessions that occurred weekly during the first year and fortnightly during the following six months. The therapist and treatment team developed a cognitive conceptualization that guided strategies for the specific interventions. At the start of therapy, Mary and her therapist collaboratively set a list of goals and began to break these goals down into concrete steps and develop a list of obstacles to those goals. Initial sessions focused on fostering engagement, improving therapeutic communication, becoming more active, and learning coping skills for auditory hallucinations.
In the middle stage of therapy, Mary learned behavioral routines—for instance, how to brew coffee and deliver it—that allowed her to begin volunteering and to develop adaptive beliefs about herself. She also corrected unhelpful paranoid thinking and broadened her coping skills for hallucinations. Toward the end of treatment, Mary practiced relapse prevention exercises, began socializing more, and generalized her volunteering to new tasks and situations. At the end of treatment and at follow-up, the phone calls had ceased, psychosocial functioning and neurocognitive performance had increased, and avolition and positive symptoms had decreased. She was not hospitalized once in 24 months.
The report, “Successfully Breaking a 20-Year Cycle of Hospitalizations With Recovery Oriented Cognitive Therapy for Schizophrenia,” is posted at http://psycnet.apa.org/index.cfm?fa=buy.optionToBuy&id=2013-34606-001.
He added that a key focus has been integrating patients into the community. “The model we have employed is a continuity-of-care approach,” he said. “We have trained providers and teams who treat these individuals in the inpatient setting as well in the community in our Assertive Community Treatment teams. Aftercare begins in the hospital, and all providers utilize the same principles: engagement, goal setting, positive action, and the removal of roadblocks to recovery.”
Grant said many patients—some of whom may have spent years in and out of hospitals—are discouraged and able to make only small progress toward their goals. “Some of them have described feeling walled off from other people and from the flow of normal human life,” he said. “Our programming teaches providers how to locate the pockets of motivation that are still available to these individuals. It helps to encourage these patients to become more active in their own recovery process. The individuals begin to dream of what they would like to do. And the challenges that they face... are addressed as solvable problems that providers work with them to neutralize as they begin to become more active and start to get back to living.”
Aaron Beck, M.D., widely known as the father of cognitive therapy, told Psychiatric News that the strategy is producing measurable results. “Our initial statistics showed a substantial decline in duration of hospitalization and a highly significant reduction in the use of restraints and seclusion,” he said. “At the same time, we worked in a short-term-care unit and similarly were able to demonstrate a substantial reduction of aggressive behavior in the unit.”
Beck added, “I think that one of the major accomplishments of our work in the community has been our ability to wed the principles of recovery to the therapeutic approaches of cognitive therapy. This has given us a very powerful instrument to counteract the hopelessness and frustration of personnel dealing with this patient population and at the same time to improve the standard of living for the patients themselves.” ■



