Controversy Follows Revelations About Nevada’s ‘Bus Therapy’ Program
Abstract
Nevada mental health officials explain why hundreds of psychiatric patients have been sent to other states with a bus ticket and a few days of medication—a policy that’s caused multiple repercussions.
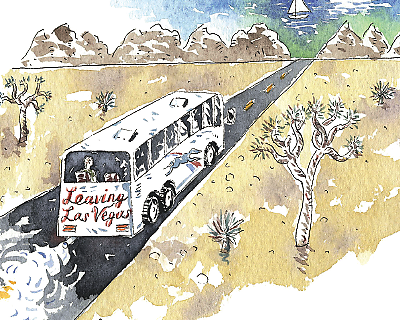
News reports and government officials have charged that beginning last March problems facing Nevada’s mental health system led to a state psychiatric hospital’s “dumping” patients into unsuspecting California localities.
The index case was that of James Brown, 48, who showed up at a social-service agency in Sacramento, Calif., with a note from the Rawson-Neal Hospital at the Southern Nevada Adult Mental Health Services in Las Vegas reading: “Discharge to Greyhound bus station by taxi with 3-day supply of medication. Follow up with medical doctor in California,” according to the Sacramento Bee.
The Bee reported that about 1,500 patients in total were discharged from Rawson-Neal to other states in the last five years. About 500 of them went to California. Nevada officials contended that most were from those other localities and could be better linked to community and family resources nearer to their places of origin.
How many patients were released as Brown was, and how many chose to go to other states is still unclear.
“People end up here and don’t want to stay here,” said Lesley Dickson, M.D., a Las Vegas psychiatrist retired from the Veterans Health Administration and a past president of the Nevada Psychiatric Association. “We all send patients home if they can go home, and patients have a role in deciding where to go.”
However, the initial uproar was enough to set off several inquiries and more. The Joint Commission investigated and withdrew the hospital’s accreditation. The Centers for Medicare and Medicaid Services placed it on warning status. Two of the hospital’s psychiatrists were disciplined.
A report requested by the Nevada governor’s office and the Nevada Department of Health and Human Services said that the hospital’s staff members “appear to be competent, compassionate, respectful, and dedicated to providing services to people with serious mental illness during the most difficult episodes of their illnesses.”
But, the report added, “discharge plans also need detailed specificity about aftercare arrangements, including the patient’s capacity to safely follow through with those arrangements.”
Ultimately, the issue moved into the courts. San Francisco’s city attorney filed suit in September demanding $500,000 in reimbursement for care for patients sent to that city. The Nevada attorney general’s office replied that 771 of the 31,000 admissions to Rawson-Neal were California residents who racked up $6.2 million in charges, implying that this was a subsidy for their West Coast colleagues.
A member of California’s congressional delegation, Doris Matsui (D), introduced a bill in the House of Representatives to create monetary penalties for any hospital or unit that fails to meet discharge standards for its psychiatric patients.
“We wouldn’t be able to comment or provide information because of pending litigation,” said Mary Woods, a public information officer at the Nevada Department of Health and Human Services, referring to the department’s “client transportation back to home communities policy.”
As has happened in other states, the number of inpatient psychiatric beds and state funding for mental health services have both dropped in Nevada in recent years.
“Salaries are way behind the national average, so doctors leave for better jobs, which leaves a bigger caseload for those who remain,” said Dickson. Staffing shortages may even be increased by one response to the crisis: requiring a staff person to accompany the discharged patients to their next destination.
The state legislature has approved $23.4 million in new funds for the state’s mental health systems.
Pressure on the state hospital also comes from emergency departments in the area’s general hospitals, which have no psychiatric wards, she said. Most patients brought in by the police go to Rawson-Neal for evaluation and stabilization, and there is a continuous need to free up beds for still more patients sent from emergency rooms.
Problems such as patient “dumping” could be reduced not only with increased mental health budgets but with interventions like “predischarge and postdischarge education, structured needs assessment, medication reconciliation and education, transition managers, and provider communication,” wrote Smita Das, M.D., Ph.D., a researcher in psychiatry and behavioral sciences at Stanford University School of Medicine, and colleagues, in a commentary in JAMA provoked by the Nevada case.
That may help in the long run, but the present is another story.
State hospitals like Rawson-Neal are placed in an impossible position by that unidirectional flow of patients, said psychiatrist Joe Parks, M.D., chief clinical officer at the Missouri Department of Health in Jefferson City.
“When psychiatric hospitals are at capacity, they can’t take new admissions or they have to let patients go prematurely or they violate their state charters or they go over census,” said Parks, speaking to Psychiatric News on behalf of the National Association of State Mental Health Program Directors. “Then they lose their certification and their funding. So pick the least bad thing and decide who’s going to get upset. That’s not a choice that allows us to do right by all policies.” ■
The “Consultation Report on Rawson-Neal Psychiatric Hospital” by Kenneth Appelbaum, M.D., and Joel Dvoskin, Ph.D., is posted at http://gov.nv.gov/uploadedFiles/govnvgov/Content/News_and_Media/Press/2013_Images/2013-05-23_ConsultationRpt_Rawson-Neal.pdf.



