Successful Public Mental Health Can’t Go It Alone
Abstract
Recovery from serious mental illness takes more than medical care; it requires social and rehabilitative services as well.
Successful community mental health requires effective partnerships and an integrated system of care bringing together primary care, mental health, and substance abuse services.
And at the level of the individual living in the community, successful recovery from serious mental illness requires more than just clinical care—it requires a range of human and social-support systems.
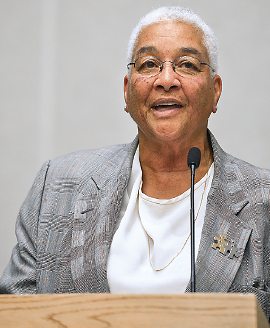
Estelle Richman says that successful community mental health services call for partnerships of key agencies, family involvement when possible, and an integrated system of care.
That’s the message Estelle Richman delivered to psychiatrists in her keynote address that kicked off this year’s APA Institute on Psychiatric Services in Philadelphia last month. During her address, she drew on her extensive background in public service and especially in closing the old Philadelphia State Hospital at Byberry (it was officially closed in 1990) and helping to build a successful community-based mental health system in the city to replace it.
“It was clear to all of us making public policy that for people with mental illness to be successful in the community, community resources needed to be expanded,” Richman said. “Some of these resources that we began to work so hard for and that we maintained a budget for were in some very concrete areas. First, housing—moving [people] from institutions to group homes to independent living with supports was the most expensive but most critical thing we could do. Housing remains a challenge for most systems.
“Work and employment are central to the growth of the individual,” she continued. “People want meaningful activities of their choice. We were quick to spot the development of day-treatment programs that offered opportunities for education and work. We worked hard to resolve homelessness, and there was a point in the 1990s when we had our homeless population [in Philadelphia] down to fewer than 200.
“We invested in teams and case management with caseloads low enough that there was time to work with clients with serious mental illness,” Richman said. “The recognition of the role of families and consumers was there in everything we did. We believed in peer support, and we believed in consumer-run services. We put our money where our mouth was, and we invested heavily.”
Richman has a long history of public service, working most recently as senior advisor to the secretary of Housing and Urban Development for health and human service issues. From 2003 to 2009, she was secretary of the Pennsylvania Department of Public Welfare. Prior to that, she was director of social services, commissioner of public health, and deputy commissioner for mental health, mental retardation, and substance abuse services for Philadelphia.
Looking back over a challenging career that has seen, as she said, “the best of times and the worst of times,” she posed the question: What does successful community mental health look like, and how will we know when we have achieved it?
She expressed optimism about the movement toward integrated care and the expansion of care, including parity coverage of mental illness/substance abuse treatment under the Affordable Care Act, but she said the vision of a truly successful mental health system has not yet been achieved.
She said, “My theme today is, ‘You’ve come a long way baby…but are we there yet?”
So, what does success look like? “Success has the following characteristics,” she said. “Teams and partnerships exist at every level. State and local governments must encourage innovation and risk-taking, stress performance-outcome measures, develop a unified-system strategy, let research drive policy and practice, and not let the perfect get in the way of the good. The federal government must be a model of collaboration for the states and must insist on partnerships between housing and health care, child welfare and health care, education, and health care. And we must find ways to integrate mental health and addiction policy.” ■



