Evidence Backs Gateway Hypothesis in Drug Addiction
Abstract
A study in mice adds insights to epidemiological research on ways in which users arrive at their drugs of addiction.
Chickens or eggs?
It’s an old argument, but addiction specialists are still scrapping over which drug of abuse users adopt first.
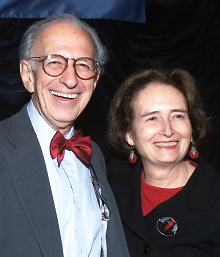
“Common factors will explain the use of drugs in general, and specific factors will explain why young people use specific drugs and do so in a particular sequence,” according to Nobel Prize–winning psychiatrist Eric Kandel, M.D., and his wife and collaborator, sociologist Denise Kandel, Ph.D., about their research on how tobacco use can serve as a “gateway” to cocaine addiction.
Do people with addiction just latch onto the first drug that comes their way, or is there a predictable escalation in their choice of substance?
“The debate is still going on,” said Denise Kandel, Ph.D., a professor of sociomedical sciences in psychiatry at Columbia University and chief of the Department of the Epidemiology of Substance Abuse at the New York State Psychiatric Institute.
Kandel is a longtime proponent of the “gateway hypothesis” of drug use: “a well-defined developmental sequence of drug use occurs that starts with a legal drug and proceeds to illegal drugs.”
Her epidemiological studies have shown that 87.9 percent of 18- to-34 year-old cocaine users had smoked cigarettes before using cocaine, but only 3.5 percent used cocaine before smoking cigarettes.
A second model of addiction posits a “common liability” to drug use—that is, an underlying general vulnerability for drug use.
Now, a combination of epidemiological and molecular research demonstrates a priming effect of nicotine on the brain that enhances the physiological response to cocaine, supporting the gateway model, according to Kandel and her husband, psychiatrist Eric Kandel, M.D., the Nobel Prize–winning professor of neuroscience and psychiatry at Columbia University and a senior investigator at the Howard Hughes Medical Institute, writing together in the September 4 New England Journal of Medicine.
“If you give an animal nicotine before you give it cocaine, it dramatically enhances the effects of cocaine, while cocaine has no effects on nicotine,” said Eric Kandel in an interview with Psychiatric News. “We showed this at the levels of gene expression and chromatin structure.”
“This is a very provocative study that asks questions with important public-health implications,” said Joni Rutter, Ph.D., director of the Division of Basic Neuroscience and Behavioral Research at the National Institute on Drug Abuse.
“In this specific drug pair, this may be a model that works,” Rutter told Psychiatric News. “It may not in other drugs of abuse, but the questions certainly could be asked. The molecular mechanisms they studied are intriguing and are certainly testable.”
Eric Kandel, his longtime collaborator Amir Levine, Ph.D., and their colleagues set out to examine several parameters of drug-use sequence.
One behavioral test, locomotor sensitization, showed that mice given nicotine in their drinking water for seven days, followed by co-administration of nicotine and cocaine for four days, displayed increased activity compared with both controls and mice getting cocaine only.
A second test, conditioned place preference, also showed that mice thus primed preferred sites associated with cocaine, compared with mice getting cocaine only.
An electrophysiologial test in the nuclear accumbens supplied more evidence.
“We found that just one injection of cocaine in a mouse given nicotine for seven days led to a marked reduction in long-term potentiation that started immediately after stimulation and persisted for up to 180 minutes,” wrote the Kandels. “Nicotine alone, cocaine alone for seven days, or seven days of cocaine followed by 24 hours of nicotine did not alter long-term potentiation.”
Finally, gene expression studies found that nicotine reduced histone deacetylase activity, thus increasing acetylation of the histones H3 and H4 at the FosB promoter in the striatum, and creating an environment conducive to FosB expression, which contributes to addictive behavior in mice.
Nicotine’s priming effect occurred only if the cocaine was first administered at the same time as nicotine, indicating that the latter may enhance the physiological effects of cocaine.
“For all the measures we studied—locomotor sensitization, conditioned place preference, long-term potentiation, and expression—reversing the order of nicotine and cocaine exposure was ineffective: cocaine did not enhance the effect of nicotine,” noted the Kandels.
“This shows that smoking is not only dangerous in its own right, but it’s capable of potentiating at least one more dangerous drug,” said Eric Kandel. “We’re now looking at whether alcohol has a similar effect or whether nicotine has similar effects on other drugs.”
The Kandels suggested that perhaps the two hypotheses about the route to addiction can be reconciled. “[W]e believe that the gateway hypothesis and the common liability model are complementary,” they concluded. “Common factors will explain the use of drugs in general, and specific factors will explain why young people use specific drugs and do so in a particular sequence.”
Their research must be replicated by independent labs but, if validated, might change the way cocaine abuse is treated, said Rutter.
“Providers treating cocaine addiction would also address nicotine use,” she said. “Nicotine replacement therapy thus might not be a good choice, and behavioral approaches might work better. The Kandels have done a nice job of setting the table for asking those kinds of questions.”
Those questions might involve gender or age, since the Kandels’ lab work was carried out only in adult male mice, she said.
Rodents starting nicotine in adolescence consume more than those who start as adults, so a study of nicotine priming should also extend to adolescents, said both Rutter and the Kandels.
“And if nicotine primes the brain for cocaine, and if that holds up in real-world settings, does it also prime for other risky, impulsive behaviors or addictions, like obesity?” she asked, referring to the fact that many women gain weight when they quit smoking.
The Kandels’ cross-disciplinary work adds new insights into the process of addiction and, if one is needed, yet another reason to keep young people from starting to smoke. ■
“A Molecular Basis for Nicotine as a Gateway Drug” can be accessed here.



