Psychiatry Match Numbers Increase Slightly
Abstract
Educational leaders worry that the increasing number of medical students needed to meet the expected physician shortage will not be coupled with a commensurate increase in residency slots.
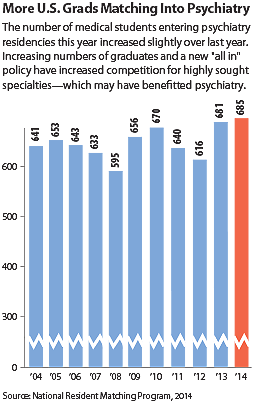
A total of 685 U.S. medical student seniors matched into psychiatry residencies in this year’s National Resident Matching Program (NRMP).
This is a small increase from 681 in 2013. The percentage of U.S. seniors selecting psychiatry (4.2 percent) is unchanged from the previous year.
This is good news for psychiatry in that it continues the reversal of a trend of several years in which the numbers were dropping; in 2012, for instance, the 616 graduates entering psychiatry represents a decrease from 640 in 2011 and 670 in 2010.
The annual match, in which the choices of graduating medical students are paired with those of residency programs, is typically watched as an indicator of workforce size and makeup of the various medical specialties for the coming years.
But a new wrinkle in the match program, introduced last year, makes the numbers slightly harder to interpret. In 2013, an “all in” policy was instituted whereby programs were required to enter all of their residency slots in the match. In past years, programs could participate in the NRMP by registering and filling some available residency positions, while also reserving some to be filled outside the match.
With the “all in” policy, there were more slots offered in the match: in 2014 the number of psychiatry slots increased to 1,322. Of those, 1,297 positions were filled in the match, with 685, or 51.8 percent, filled by U.S. seniors. As in past years, positions not filled by U.S. seniors were filled by international medical graduates (including U.S. and non-U.S. citizens), Canadian students, students of osteopathic schools, and individuals who graduated from medical school in previous years.
Psychiatric educators’ concern for the future is based not only on the match results but also on the expected increase in the number of medical school graduates coupled with the absence of a commensurate increase in residency positions and the ongoing cap on funding of residencies by the Medicare program. The number of medical students is on the rise to meet the forecast physician shortage.
Former APA Trustee Sidney Weissman, M.D., explained that the number of U.S. seniors obtaining positions in the match rose from 14,992 in 2010 to 16,399 in 2014, paralleling the increase in U.S. medical graduates. “It is anticipated that in 2018 we will have 20,055 allopathic seniors and 2,600 osteopathic seniors in the match,” he said. “These combined numbers will exceed the total number of first-year positions offered in the 2014 match—26,678.
“With the number of residency positions funded by Medicare capped, we will see an increasing number of U.S. seniors unable to obtain residency positions,” Weissman told Psychiatric News. “If we are to effectively expand the number of practicing physicians at a time of growing shortage, it is critical that government funding be made available to support growth in the number of residency positions.
“While the total number of U.S. medical students is increasing, it is not likely that the total number of psychiatry residency positions will be altered significantly without major changes in government policy,” Weissman said. “This is the time for psychiatry to reassess what the core or basic training in psychiatry should be for all medical students. This is critical for our recruiting new psychiatrists as well as in the training of other physicians, all of whom provide essential mental health care.”
Weissman is not alone in his concern about the future of residency and federal funding for graduate medical education. In a statement issued with the release of the match numbers, Darrell Kirch, M.D., president and CEO of the Association of American Medical Colleges (AAMC), said that a preliminary analysis of this year’s data shows that several hundred U.S. medical students did not match to a first-year residency training program.
“As a result, with a serious physician shortage looming closer, we remain concerned that the 17-year cap on federal support of new doctor training will impede the necessary growth in residency positions that must occur to ensure that our growing and aging population will receive the care it needs,” Kirch said. “According to the most recent AAMC Survey of Medical School Enrollment Plans, U.S. medical school enrollment will increase to 21,349 students by 2018. Combined with the larger number of graduates from osteopathic schools, which also are expanding to address the shortage, as well as increasing numbers of international graduates entering the match, there may be too few residency positions for all the newly graduated doctors in the not-too-distant future.” ■
Preliminary data from the NRMP can be accessed here.



