Same Brain Circuits Linked With Psychosis in Two Disorders
Abstract
The brains of schizophrenia patients and of those with bipolar disorder who experience psychotic episodes show similar connectivity patterns, which points to a common mechanism that may be associated with psychotic symptoms in the two disorders.
Why is it that some individuals with bipolar disorder experience psychotic episodes, whereas others do not? It could be because the former have certain brain abnormalities in common with individuals who have schizophrenia, a new study suggests.
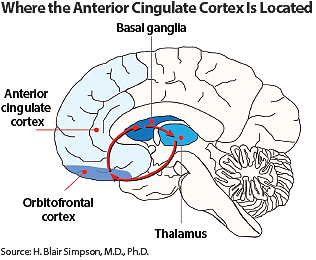
The abnormalities concern the ventral anterior cingulate cortex (vAAC), a region in the prefrontal cortex thought to regulate emotional behavior through nerve connections with other areas of the brain—notably the orbitofrontal cortex, insula, amygdala, and hypothalamus.
The lead researcher was Alan Anticevic, Ph.D., an assistant professor of psychiatry and psychology at Yale University. The results were published April 29 in Schizophrenia Bulletin.
Many individuals with bipolar disorder also experience psychotic episodes. Functional disturbances in prefrontal cortex regions of the brain involved in affect and mood regulation—especially the vAAC—have been implicated in several bipolar disorder studies. Thus Anticevic and his team wanted to determine whether the vAAC might play a role in bipolar-related psychosis.
Their cohort included 202 subjects—40 with bipolar disorder who were currently experiencing neither depression nor mania and who had never experienced psychotic episodes; 33 with bipolar disorder who were currently experiencing neither depression nor mania but who had experienced psychotic episodes; 56 demographically matched healthy controls, and 73 demographically matched subjects with schizophrenia. The researchers used brain imaging to compare the functional connectivity of the vAAC among the four subject groups.
Compared with the control subjects, the bipolar-without-psychosis group showed significantly increased coupling of the vAAC to other brain regions, whereas the bipolar-with-psychosis subjects showed significantly decreased coupling of the vAAC to other brain regions. Moreover, the vAAC connectivity observed in schizophrenia subjects was significantly different from that found in the bipolar-without-psychosis subjects, but similar to that found in the bipolar-with-psychosis subjects. The findings remained the same even when the medications that subjects were using were taken into consideration.
“The similarities in vAAC connectivity patterns in schizophrenia and psychotic bipolar disorder patients may suggest the existence of common mechanisms underlying psychotic symptoms in the two disorders,” Anticevic and his colleagues concluded.
And these findings may have research implications, they noted, suggesting that researchers should “study neural circuit alterations across neuropsychiatric diagnoses, rather than studying narrowly predefined diagnostic categories.”
“The findings reported here are striking and may be very important,” J. Raymond DePaulo Jr., M.D., a professor of psychiatry at Johns Hopkins University and a bipolar disorder expert said in an interview with Psychiatric News. “The findings are a step toward making functional sense of some of psychiatry’s diagnostic groupings and, if confirmed and extended, would contribute to the scientific substrate from which laboratory methods could be introduced into the psychiatric assessments of the future.”
The research was funded by the National Institutes of Health, the Fulbright Foundation, and the Brain and Behavior Research Foundation. ■
An abstract of “Ventral Anterior Cingulate Connectivity Distinguished Nonpsychotic Bipolar Illness From Psychotic Bipolar Disorder and Schizophrenia” can be accessed here.



