APA Task Force to Address ‘What’s Next?’ for Ketamine
Abstract
One expert recommends that patients be referred for ketamine treatment only after they have failed all approved appropriate treatments, including ECT.
It has been more than 15 years since researchers first discovered that a single infusion of the anesthetic ketamine could reduce symptoms of depression in a fraction of the time it typically takes a standard antidepressant to take effect. As more evidence has pointed to ketamine’s efficacy in patients who have failed to respond to other depression treatments, the number of those seeking the medication have grown.
Despite all of the excitement over ketamine’s antidepressant properties, however, experts warn that serious questions about the medication remain.
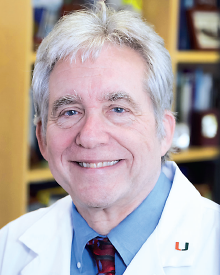
“We are in the unusual situation where ketamine is readily available, but there is little clinical-trial data to drive practice.”
“We are in the unusual situation where ketamine is readily available, but there is little clinical-trial data to drive practice,” said Charles Nemeroff, M.D., Ph.D., the Leonard M. Miller Professor and chair of the Department of Psychiatry and Behavioral Sciences at the University of Miami Miller School of Medicine. “There are a number of questions: What kind of psychiatric screening should be done in potential patients? How should a patient be monitored? What kind of follow-up should take place after treatment?”
To begin to answer these questions, the APA Task Force on Novel Biomarkers and Treatments scrutinized the literature for placebo-controlled, double-blind, randomized clinical trials that examined ketamine and other N-methyl-d-aspartate (NMDA) antagonists in the treatment of depression.
The results of the group’s meta-analysis, which appeared October 1 in the American Journal of Psychiatry, focused on 12 clinical trials; seven (including 147 ketamine-treated participants) evaluated ketamine’s effectiveness as a monotherapy or in combination with other psychotropic medications, and five (including 89 ketamine-treated patients) evaluated whether the medication might augment electroconvulsive therapy (ECT).
The analysis confirmed that a single intravenous infusion of ketamine consistently produced a rapid and robust antidepressant effect that peaked within 24 hours of administration, accompanied by brief psychotomimetic and dissociative effects. However, within one week, these antidepressant effects were largely diminished. Additionally, while ketamine accentuated the antidepressant effects of ECT following an initial treatment, it did not have any significant effect at the conclusion of the ECT treatment regimen.
“[The] current data provide compelling evidence that the antidepressant effects of ketamine infusion are both rapid and robust, albeit transient,” Nemeroff, chair of the task force, and colleagues wrote.

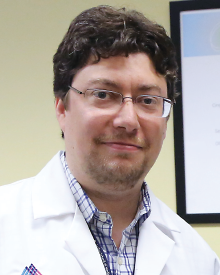
Carlos Zarate Jr., M.D., points out that the patients who responded to a single infusion of ketamine for up to a week were very sick.
While the meta-analysis adds further evidence confirming ketamine’s rapid antidepressant effect, Carlos Zarate Jr., M.D., chief of the Experimental Therapeutics and Pathophysiology Branch of the Division of the Intramural Research Program at the National Institute of Mental Health, told Psychiatric News that more research is needed to establish how long or short term these effects might be.
“It is important to remember that we are talking about very sick patients who responded to a single infusion of ketamine for up to a week,” said Zarate, who led several of the ketamine trials included in the task force meta-analysis but was not involved with the current study. “In the studies performed by our group, the majority of patients had failed six or more antidepressant trials. … No chronic condition gets better with one dose [of treatment].”
Recent preliminary data suggest that multiple doses of ketamine are associated with rapid and sustained improvements in mood, Zarate said.
Still, there are concerns over the abuse liability of ketamine—the drug is sought after for recreational use for its ability to produce “out-of-body” experiences and hallucinations. Preclinical trials suggest that the drug may also be neurotoxic if administered at high doses or over extended periods. Additionally, Nemeroff noted, much is unknown about the precise mechanism of ketamine’s antidepressant effects.
The task force also analyzed the findings of several randomized, controlled trials of other NMDA antagonists, including lanicemine, memantine, and nitrous oxide, and two partial agonists at the NMDA coagonist site, d-cycloserine and rapastinel. They found that while lanicemine, memantine, and nitrous oxide—which bind to the receptor at the same site as ketamine—failed to demonstrate efficacy consistently, d-cycloserine and rapastinel significantly reduced depressive symptoms without psychotomimetic and dissociative effects.
“It is important to hone in on mechanism of action, what’s responsible for ketamine’s side effects and what’s responsible for its antidepressant effects,” Zarate said. He and his colleagues are searching for biomarkers that identify individuals most likely to respond to ketamine; they are also studying other medications that modulate NMDA receptors. Such information could one day guide the development of “safer, ketamine-like drugs,” he added.
James Murrough, M.D., asks that for those patients who respond quickly to ketamine, what should the next step be in their treatment?
“The evidence is now pretty clear that low-dose ketamine can have a meaningful antidepressant effect with a rapid onset of action,” James Murrough, M.D., an assistant professor of psychiatry and neuroscience at Mount Sinai School of Medicine, told Psychiatric News. “If patients do respond, then the question becomes, again, ‘What’s next?’ ”
This is one of the questions that Nemeroff hopes the task force may be able to answer as they begin to work on developing a set of treatment recommendations for ketamine based on the information that is now available. “There is a pressing need to provide treatment recommendations for use of ketamine right now,” he said.
Nemeroff noted that when faced with a patient with treatment-resistant depression, it is first important to verify the patient has tried and failed to respond to FDA-approved antidepressant treatments and other evidence-based “tried and true” treatment strategies before considering ketamine.
“If someone has received all treatments possible without success, including ECT,” Nemeroff said, “only then would I refer the patient to one of the academic centers with specialized treatment-resistant depression clinics that are currently conducting ketamine trials.” ■
“Ketamine and Other NMDA Antagonists: Early Clinical Trials and Possible Mechanisms in Depression” can be accessed here.



