CBT May Lead to Longer-Lasting Improvements For Patients With SAD
Abstract
Patients with seasonal affective disorder who received six weeks of cognitive-behavioral therapy were less likely than those who receive light therapy to see their symptoms return two years later.
Light therapy is an effective treatment for acute seasonal affective disorder (SAD), but less is known of the therapy’s long-term effectiveness, as patients often forget to resume their light therapy in subsequent winters or fail to maintain a consistent, daily routine.
An alternative treatment option is a form of cognitive-behavioral therapy tailored for SAD (CBT-SAD), which was recently shown to be as effective as light therapy in alleviating depression associated with SAD (Psychiatric News, May 15).
Although CBT-SAD requires a greater investment from patients upfront—instead of 30 minutes in front of a light box each day, participants engage in weekly sessions with a therapist and complete homework assignments—a study published November 5 in AJP in Advance suggests CBT-SAD may offer more long-term durability.

Kelly Rohan, Ph.D., has developed a version of cognitive-behavioral therapy for seasonal affective disorder (SAD) that has shown efficacy and durability in reducing depressive symptoms, and she believes it offers another proven treatment option for patients with SAD.
Kelly Rohan, Ph.D., a professor of psychological science at the University of Vermont and the developer of CBT-SAD, and colleagues randomly assigned 177 participants with SAD to receive CBT-SAD (two 90-minute sessions per week) or light therapy (30 minutes each morning) for six weeks. The participants were then assessed one and two winters later.
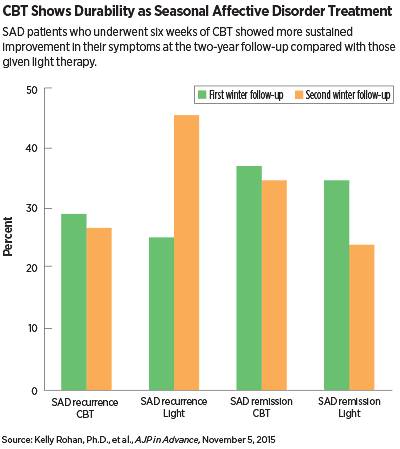
In the first follow-up winter, the recurrence of SAD was about the same in the two groups (28.9 percent recurrence rate for CBT-SAD and 24.9 percent for light therapy). During the second winter, however, CBT-SAD had a 27.3 percent recurrence rate compared with 45.6 percent for light therapy.
When the researchers examined the patient characteristics in between the first and second winters, they found that CBT-SAD participants who did not have a recurrence during the first winter were five times as likely to stay symptom-free the following winter, whereas successful light therapy participants were only twice as likely to not have a recurrence.
A similar pattern of durability emerged for SAD remission, with similar rates for the therapies in the first winter (37 percent for CBT-SAD and 34.2 percent for light therapy, as measured by the Structured Interview Guide for the Hamilton Depression Rating Scale) and a stronger showing for behavioral therapy in the second year (34.1 percent for CBT-SAD and 22.9 percent for light therapy).
“The good news of these findings is that there are two proven options to treat seasonal affective disorder,” Rohan told Psychiatric News. She does not think CBT-SAD should yet be called a preferred treatment, given that the two approaches operate on quite distinct mechanisms.
“Data show that SAD patients have a more external worldview, that outside forces are in control of their mood. That is why many patients respond to a light box, which is a medical device that changes these external factors,” she explained. “CBT is an internal approach that requires patients to think outside the light box and appreciate that their depressive mood comes from within and that they can change their behavior.”
Rohan noted these two different mindsets may explain one of her previous studies that found a combination of CBT-SAD and light therapy was less effective for acute SAD than CBT-SAD by itself.
Norman Rosenthal, M.D., a clinical professor of psychiatry at Georgetown University School of Medicine, who first described SAD and pioneered the use of light therapy, agrees that both techniques have a place in the treatment of this disorder. Rosenthal was not involved with this study.
“Importantly, this work shows the value of teaching people about their illness and what they can do to change their behavior,” he told Psychiatric News. “It reminds me of a SAD program I had at NIMH many years ago in which we surveyed patients as to what they believed was most critical to their improvement. I thought that the light boxes would come out on top, but the patients stressed education about their illness.”
Rosenthal believes that educating SAD patients about their illness, its course, and treatment options is valuable regardless of the treatment regimen used. “Clinicians do not have to go the full extent of CBT, but they could incorporate elements of cognitive and behavioral modification to someone taking light therapy or medication, and that could help them stay compliant.”
Rohan hopes to address that very question in a project she’s putting together now, which will involve providing some “booster sessions” to patients in the autumn to see if that improves winter outcomes; for CBT-SAD participants, it would entail short sessions reminding them how to use the CBT skills they’ve learned, while light therapy participants would receive some motivational interviewing to keep them on the proper routine.
Rohan’s study was supported by a grant from the National Institute of Mental Health and the Mental Illness Research, Education and Clinical Centers. ■
“Outcomes One and Two Winters Following Cognitive-Behavioral Therapy or Light Therapy for Seasonal Affective Disorder” can be accessed here.



