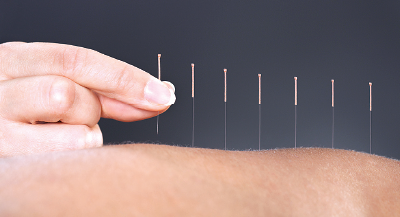
Acupuncture for Depression: Pros, Cons, and Other Sticking Points
Abstract
While the lack of an effective placebo control will likely prevent solid evidence of efficacy, acupuncture may be a viable option for some patients.
Albert Yeung, M.D., sees both the promise and limitations of acupuncture to help treat people with psychiatric issues such as depressed mood, fatigue, or insomnia.
Yeung said that while many patients have told him that acupuncture helped them to feel better, tracking down evidence to support these reports can be challenging.
There have been dozens of studies evaluating the effectiveness of acupuncture alone or in combination with medications to treat mood disorders in the past few years. And at first glance, many of them appear to provide evidence that acupuncture is a promising treatment option.
For example, a meta-analysis that included 13 trials and over 1,000 patients with depression found that combining acupuncture with selective serotonin reuptake inhibitors (SSRIs) improved average therapeutic response by about 20 percent over the first six weeks compared with SSRIs alone. This research was published in the November 2015 issue of the Journal of Affective Disorders.
“Upon closer examination, however, these studies have several limitations that make the data inconclusive,” said Yeung, the director of Primary Care Research at the Depression Clinical and Research Program at Massachusetts General Hospital.
As Yeung explained, the nature of acupuncture is such that it’s nearly impossible to design any definitive clinical comparison studies. For starters, acupuncture is highly individualized when considering the background and technique of the practitioner and the exact symptom presentation of the patient.
Another problem is there is no way to create a good placebo with which acupuncture can be compared. Sticking people with needles in nonacupuncture points is not ethical, and even if it were, the needle would still induce the release of the body’s endorphins, which contribute some of the positive effects of acupuncture. In contrast, sham needles—blunt devices that press against the skin but then retract—are only moderately effective at simulating acupuncture.
“Anyone with even limited acupuncture experience should be able to tell the difference” between sham and real needles, Yeung said.
With these drawbacks, as well as the fact that most clinical trials involve only small numbers of participants, it is not surprising that both the APA Practice Guidelines for the Treatment of Patients With Major Depressive Disorder and a Cochrane review on acupuncture for depression—both published in 2010—do not recommend acupuncture as a treatment option for people with depression.
In response to the Cochrane review, Hugh MacPherson, Ph.D., a senior research fellow of health sciences at the University of York in England and acupuncturist, carried out a large randomized trial comparing acupuncture with other structured therapies like counseling.
The results of this trial suggested that incorporating regular sessions of either acupuncture or humanistic counseling, which aims to help people realize their potential and creativity, improved depressive symptoms in the participants after 12 months when compared with usual care alone (medication or psychiatric referral), with the two approaches showing similar improvement levels.
“Acupuncture and counseling were also both cost-effective when considering improvements in the patients’ quality of life in relation to the extra costs,” MacPherson said.
As Yeung pointed out, since the publication of the APA practice guideline and Cochrane review years ago, there has been growing recognition that activities such as yoga, meditation, and acupuncture can provide some psychological benefits with a minimal side effects.
“More and more psychiatrists may find their patients asking about acupuncture or related natural therapies, so they should be aware of both the potential limitations and costs involved,” Yeung told Psychiatric News. ■
An abstract of “The Benefit of Combined Acupuncture and Antidepressant Medication for Depression: A Systematic Review and Meta-Analysis” can be accessed here. “Cost-Effectiveness Analysis of Acupuncture, Counselling, and Usual Care in Treating Patients With Depression: The Results of the ACUDep Trial” is available here.



