AMA Calls on Licensing Boards to End Discrimination for MH Treatment
Abstract
AMA delegates acted on resolutions focused on gender disparities in mental health treatment, the mental health of medical students and residents, and expansion of availability of buprenorphine.
The AMA is encouraging state medical boards to recognize that the presence of a mental health condition “does not necessarily equate with an impaired ability to practice medicine.”
Psychiatrist Barbara Schneidman, M.D., a past president of the Federation of State Medical Boards, emphasizes that boards should focus only on current impairment, not past treatment, in evaluating candidates for licensure.
At the AMA House of Delegates’ annual policymaking meeting last month in Chicago, the 500-plus members all but unanimously approved a resolution encouraging state licensing boards to “consider physical and mental conditions similarly” in the evaluation of applications for medical licensure and to focus on current impairment rather than past treatment. The resolution was brought to the House of Delegates by the AMA’s Resident and Fellow Section.
The licensure resolution was one of several focused on mental health—especially the mental health of students and trainees—during a meeting in which delegates also struck back at the Republican-led health reform effort and immigration policies of President Donald Trump.
“This is an issue of stigma against mental illness,” said Claudia Reardon, M.D., a member of the AMA Section Council on Psychiatry, during hearings on the resolution. “We should not be asking questions on medical licensing applications that are different when it comes to mental illness from those regarding general medical illnesses. … [W]hat matters is whether there is current functional impairment.”
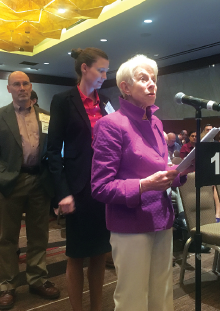
Barbara Schneidman, M.D., also a member of the section council and a past president of the Federation of State Medical Boards, said she hopes that the AMA resolution will be a “first step” in rectifying a licensure application process that has historically discriminated against individuals who have been treated for mental illness or substance use disorders. As a model for all state licensing boards, she presented to the House APA’s 2015 Position Statement on Inquiries About Diagnosis and Treatment of Mental Disorders in Connection With Professional Credentialing and Licensing.
In addition to a set of recommended guidelines for licensing boards, the APA statement notes that “[t]he salient concern for licensing entities is always the professional’s current capacity to function and/or current functional impairment. Questions on application forms should inquire only about the conditions that currently impair the applicant’s capacity to function as a licensee and that are relevant to present practice.”
The APA position statement provides the following as examples of questions that might be asked:
Are you currently using narcotics, drugs, or intoxicating liquors to such an extent that your ability to practice [law/medicine/other profession] in a competent, ethical, and professional manner would be impaired? (Yes/No)
Are you currently suffering from any condition that impairs your judgment or that would otherwise adversely affect your ability to practice [law/medicine/other profession] in a competent, ethical, and professional manner? (Yes/No)
“APA recognizes the important role served by licensing boards in protecting the public and may inquire about current functional impairment in professional conduct and current general medical or mental disorders that may be associated with such impairment,” Schneidman told physicians at the AMA meeting. “But APA believes that prior diagnosis and treatment of a mental disorder are not relevant to current impairment, and oversight entities should not include questions about past diagnosis and treatment of a mental disorder.”
The licensing resolution is a reflection of growing awareness of the mental health needs of students, trainees, and young physicians and increasing concern about untreated mental illness among students and residents facing mounting educational debt and burnout.
Between 300 and 400 physicians die by suicide each year, according to a 2015 study in JAMA Psychiatry. That same study concluded that “trainee depression and suicide are well-known concerns in the medical community that have not yet been adequately addressed.”
Citing those statistics and acknowledging barriers to accessing care, AMA delegates also adopted a new policy encouraging the study of “medical student mental health, including but not limited to rates and risk factors of depression and suicide.” The policy also encourages medical schools to confidentially gather and release information on reporting rates of depression and suicide on an opt-out basis.
AMA delegates also approved resolutions on the following mental health topics:
Women’s mental health: Calls on the AMA to work with other organizations to identify barriers in access to mental health services and improve treatment models to address gender disparities in mental health and to publicize the impact of violence and social determinants on women’s mental health. The resolution further advocates for inclusive insurance coverage of mental health services during gestation and extension of postpartum mental health services coverage to one year postpartum.
Supervised injection centers: Supports the development and implementation of pilot supervised injection facilities (SIFs)—centers where individuals addicted to heroin or other injectable drugs may inject under medical supervision. Delegates testified that evidence from Europe where such centers are legal shows that individuals who visit SIFs are more likely to safely inject and more likely to enter into treatment. The resolution states that such pilot programs should be “designed, monitored, and evaluated to generate data to inform policymakers on the feasibility, effectiveness, and legal aspects of SIFs in reducing harms and health care costs related to injection drug use.”
Expanding availability of buprenorphine: Directs the AMA’s Opioid Task Force to publicize existing resources that provide advice on overcoming barriers and implementing solutions for prescribing buprenorphine for treatment of opioid use disorder. ■
“Depression and Suicide Among Physician Trainees: Recommendations for a National Response” can be accessed here.



