Researcher Discusses Goals and Challenges of Perinatal Mental Illness
Abstract
Katherine Wisner, M.D., a pioneer in the area of perinatal mental health, says the paucity of clinical studies on pregnant women makes it difficult to weigh the risks of mental illness against the risks of medication treatment.
Katherine Wisner, M.D., the recipient of APA’s 2017 Award for Research in Psychiatry, considers pregnant women to be the last therapeutic orphans of modern medicine.
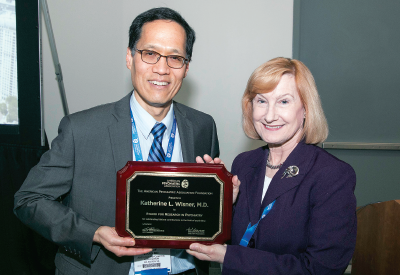
Philip Wang, M.D., Ph.D., director of APA’s Division of Research, presents Katherine Wisner, M.D., with APA’s 2017 Award for Research.
Today, most everyone acknowledges that pregnant women get sick, and sick women get pregnant, Wisner told an audience during the award lecture at APA’s 2017 Annual Meeting.
However, it was once believed that pregnancy protected women from illness, especially mental illness, said Wisner, the Norman and Helen Asher Professor of Psychiatry and Behavioral Sciences and Obstetrics and Gynecology at Northwestern University Feinberg School of Medicine.
Wisner recalled a conversation durig her residency in an obstetrics ward with a supervisor about a patient who showed telltale signs of depression.
“My supervisor dismissed the idea, for she told me, ‘She cannot be depressed, because she is pregnant, and pregnant women are fulfilled.’”
But among the many health risks facing women during pregnancy, mental illnesses such as depression and bipolar disorder are some of the most common and debilitating to both mother and child.
“We hear a lot about the many risks of maternal mental illness on childbirth, but mental illness also affects the maternal ability to nurture the infant over time,” Wisner said. “And that leads to long-term developmental impairments in the child.”
Wisner has dedicated her career to understanding the complex effects of psychiatric illness during the perinatal period and has provided tremendous insight into the prevalence of these problems as well as the effects of psychotropic treatments during pregnancy.
The benefits and risks of medication during pregnancy, particularly antidepressants, has garnered much attention in the news over the past few years, Wisner noted during the lecture. But conflicting and ambiguous data from recent studies have led to confusion and doubt among clinicians and their pregnant patients.
Wisner noted that the actual data on how medications such as antidepressants affect pregnancy are sparse, since pregnant women are often excluded from clinical trials. Most findings come from retrospective, population analyses of mothers following birth—the kind of studies where sampling biases or other external factors can readily influence results.
“Both major depressive disorder and antidepressants can impact maternal, fetal, and infant outcomes,” she said. However, other confounders, including medical comorbidity, poor nutrition, and substance use, can also influence outcomes.
Obesity is one such confounding factor, Wisner explained, as she discussed concerns linking antidepressants to an increased risk of birth defects. Wisner noted that it is not widely appreciated that obesity is associated with birth defects like spina bifida or congenital heart defects, and depressed women tend to have a higher risk of being overweight or obese.
“Even if the depression or medication underlies some of the risk, these birth defects are pretty rare, and the absolute risk is low,” a point often downplayed in studies exploring these risks and the media coverage of such studies, she said.
That is not to suggest that potential risks should be discounted; physicians should be aware of all potential benefits and risks when prescribing to a pregnant woman, Wisner said. And uncovering those risks will require addressing some fundamental questions.
“We still don’t know how to optimally treat pregnant women,” she said. “What are the ideal doses? Research has shown that plasma concentrations of antidepressants seem to drop over the course of pregnancy, so adjustments are needed.”
Wisner hopes to answer these and other questions with her latest project, a National Institute of Child Health and Human Development–funded study called OPTI-MOM. This study is enrolling 200 pregnant women with depression who are taking antidepressants and sequencing their genetic data on drug metabolizing enzymes. Wisner’s team will periodically take blood samples from the women during the course of pregnancy and analyze the concentrations of antidepressants in these women of differing metabolic profiles.
The findings may lead to the development of tailored treatment algorithms for antidepressants during pregnancy, which will be one more important step to finding these therapeutic orphans a home. ■



