Med Check
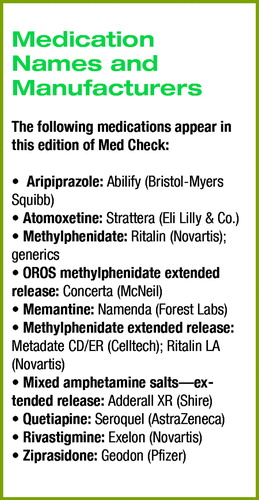
This is the first of a two-part edition of Med Check, featuring new research abstracts presented at APA's 157th Annual Meeting in New York City in May. This part covers research relating to medication treatment of ADHD, Alzheimer's disease and other dementias, and bipolar disorder. The second part will cover pharmacotherapy of depression and anxiety, psychotic disorders, and sleep disorders.
The research presented in this format is preliminary, has not been published in a peer-reviewed journal, and may involve uses of medications for purposes that are not FDA approved. New research abstract reports are largely sponsored by the products' manufacturers.
Attention-Deficit/Hyperactivity Disorder (ADHD)
• Atomoxetine is associated with fewer sleep disturbances than methylphenidate in children with ADHD. A Lilly-funded, double-blind, randomized study looked at 85 patients taking the two drugs over 16 weeks in a crossover design. Patients took either atomoxetine or methylphenidate for seven weeks, followed by a 10- to 20-day drug-free phase. Then patients crossed over to the opposite drug for seven weeks. Sleep assessments included actigraphy, polysomnography (on a subset of patients), and parent and child diaries.
Patients taking atomoxetine experienced shorter time to sleep onset, longer actual sleep time, and fewer sleep-related problems. Results were consistent across the different measures.
APA: NR496. Presented May 4, 2004.
• Atomoxetine is effective in improving ADHD symptoms in a real-world setting, according to data from the first prospective, observational, longitudinal, open-label study of the drug's effects. Data were collected on 482 pediatric patients during routine physician visits; drug administration and dosing were at the physician's discretion. Using the Physician Global Impression: ADHD Severity scale as well as parent rating reports, researchers found that atomoxetine improved ADHD symptoms throughout the day and into the evening for many patients. Improvement was observed in core symptoms, overall behavioral assessment, and family interactions and was consistent between patients who had never taken ADHD medication prior to the study and those who had previously taken stimulants.
APA: NR475. Presented May 4, 2004.
• Mixed amphetamine salts–extended release is associated with significantly greater improvement in school performance in children aged 6 to 12, compared with atomoxetine. In a large, Shire-funded, classroom-based study, children taking either medication improved on measures of behavior, attention, and academic productivity. However, those taking mixed amphetamine salts–extended release consistently showed greater improvement in all three areas, compared with those on atomoxetine throughout a 10- to 12-hour classroom day. Side effects were mild to moderate and consistent with those known with the two medications.
APA: NR450. Presented May 4, 2004.
• OROS methylphenidate may provide better symptom relief than atomoxetine, according to data from a McNeil-funded study of more than 1,300 children between the ages of 6 and 12. Preliminary results for the first half of patients completing the three-week, open-label, parallel-design study showed an early and consistent advantage for those taking OROS methylphenidate. Based on ratings with the Attention-Deficit/Hyperactivity Disorder Rating Scale, patients taking OROS methylphenidate improved by 11.5 points by the end of the first week, while those taking atomoxetine, on average, improved 8.5 points.
By the end of the third week, patients taking OROS methylphenidate had an average score reduction of 21.1 points, compared with 15.9 points for those taking atomoxetine. Treatment-emergent adverse effects were similar in both groups and consistent with the two medications' experience. APA: NR451. Presented May 4, 2004.
Alzheimer's Disease and Other Dementias
• Memantine is safe and well tolerated in both short-term and long-term treatment of dementia, according to a pooled analysis of 940 patients treated with the NMDA receptor antagonist, compared with 922 patients treated with placebo.
In short-term trials (fewer than 28 weeks) only headache and confusion were reported in more than 5 percent of patients taking memantine and at a rate at least twice that of placebo. Agitation, diarrhea, accidental injury, and urinary incontinence were reported in more than 5 percent of patients taking memantine; however, these rates were significantly lower than those of the corresponding placebo groups. In longer-term extension trials (up to two years) agitation and urinary tract infection were the most frequently reported adverse events, though rates were indistinguishable between those of memantine and placebo. APA: NR831. Presented May 6, 2004.
• Rivastigmine appears to slow the progression of Alzheimer's disease for as long as five years. Pooled long-term data from studies evaluating more than 2,000 patients on the acetylcholinesterase inhibitor for more than five years demonstrate a significant decrease in the rate of decline, compared with projected declines in cognitive domains if the same patients had not been on medication. Using the Alzheimer's Disease Assessment Scale (ADAS-cog) patients at the beginning of their five years of rivastigmine therapy had an average score of 17.4. By the end of the study, those patients had, on average, declined to an average score of 36.8 (higher numbers indicate more cognitive dysfunction). In comparison, those same patients would have been projected to decline to an average score of 56.9 if they had not taken any medication. Overall, rivastigmine was associated with delaying a patient's decline into severe dementia by at least two years. APA: NR501. Presented May 4, 2004.
Bipolar Disorder
• Aripiprazole is safe and effective in the treatment of patients with acute manic and mixed episodes associated with bipolar disorder. A phase III, multicenter, double-blind, placebo-controlled study evaluated a 30 mg dose over a three-week period in 272 patients with bipolar I disorder. By day four, patients taking aripiprazole had an average 12.5 point improvement on the Young Mania Rating Scale, compared with a 7.2 point improvement for those taking placebo. Adverse effects seen in the aripiprazole group at a rate of at least 10 percent and twice that seen in the placebo group included stomach upset, constipation, akathisia, and pain in the extremities.
A second analysis pooled data from four separate multicenter trials comparing aripiprazole with placebo in nearly 1,000 patients. In this analysis, there was no statistically significant weight gain seen with aripiprazole, compared with placebo, and no dose-dependent differences in extrapyramidal adverse events. The most frequently reported adverse events were headache, nausea, dyspepsia, agitation, and akathisia.
APA: NR742, NR746. Presented May 5, 2004.
• Quetiapine is safe and effective for the treatment of patients experiencing acute manic episodes associated with bipolar I disorder. Remission rates were compared after three weeks and at the end of a 12-week, double-blind, placebo-controlled study, with remission defined as a Young Mania Rating Scale score of 12 or less. For patients taking quetiapine, 37.5 percent achieved remission by day 21 and 65.4 percent by day 84. In comparison, only 23 percent of those taking placebo achieved remission by day 21 and 35.9 percent did so by day 84. The most frequently encountered adverse events noted with quetiapine are somnolence, dry mouth, dizziness, constipation, asthenia, abdominal pain, changes in liver function, and weight gain. APA: NR 752. Presented May 5, 2004.
• Ziprasidone provides rapid and significant improvement in patients with acute bipolar mania. A pooled analysis of two randomized, double-blind studies involving 415 patients hospitalized for acute mania showed that improvement was evident as early as the second day, and consistent improvement continued over the course of the three-week studies.
Ziprasidone was equally effective in patients with manic or mixed episodes and in those with or without psychotic symptoms. Dosing started at 80 mg per day and was titrated up to 160 mg per day by the second or third treatment day. The most common side effects were somnolence, headache, and dizziness.
In a second study—a one-year, open-label, extension study—ziprasidone continued to improve manic symptoms, with no increases in weight, cholesterol, or triglycerides. APA: NR777, NR745. Presented May 5, 2004.



