Long-Term Data Document Course of BPD Symptoms
Borderline personality disorder (BPD) appears to comprise symptoms that are manifestations of acute illness as well as symptoms that represent more enduring aspects of the disorder.
The former are akin to the positive symptoms of schizophrenia and the latter are akin to the negative symptoms of schizophrenia, according to a longitudinal study of BPD patients in the June American Journal of Psychiatry.
Researchers assessed the borderline psychopathology of 362 patients with personality disorders using two semistructured interviews of proven reliability.
All patients were recruited during inpatient stays.
Of these, 290 patients met DSM-III-R criteria as well as Revised Diagnostic Interview for Borderlines criteria for BPD, and 72 met DSM-III-R criteria for another Axis II disorder. Over 85 percent of the patients were interviewed again at five distinct two-year follow-up waves by interviewers blind to all previously collected information.
Twenty-four symptoms were studied at baseline and follow-up (see table).
Twelve of the 24 symptoms studied showed patterns of sharp decline over time and were reported at 10-year follow-up by less than 15 percent of the patients who reported them at baseline. The other 12 symptoms showed patterns of substantial but less dramatic decline over the follow-up period.
Symptoms reflecting core areas of impulsivity (such as self-mutilation and suicide efforts), and active attempts to manage interpersonal difficulties (such as problems with demandingness/entitlement and serious treatment regressions) seemed to resolve the most quickly.
In contrast, affective symptoms reflecting areas of chronic dysphoria (such as anger, loneliness, or emptiness) and interpersonal symptoms reflecting abandonment and dependency issues (such as intolerance of aloneness and problems with dependency) seemed to be the most enduring.
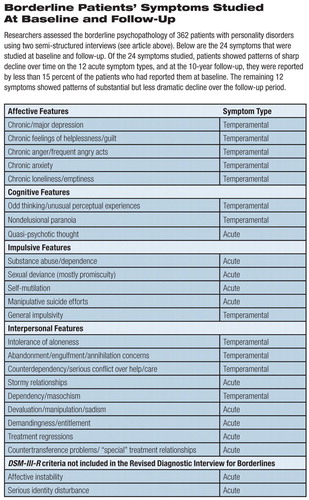
Borderline Patients' Symptoms Studied at Baseline and Follow-Up
Researchers assessed the borderline psychopathology of 362 patients with personality disorders using two semi-structured interviews. (see article above) Below are the 24 symptoms that were studied at baseline and follow-up. Of the 24 symptoms studied, patients showed patterns of sharp decline over time on the 12 acute symptom types, and at the 10-year follow-up, they were reported by less than 15 percent of the patients who had reported them at baseline. The remaining 12 symptoms showed patterns of substantial but less dramatic decline over the follow-up period.
Lead author Mary Zanarini, Ed.D., told Psychiatric News that many of the patients received treatment over time, but as the study was naturalistic, they were not randomized to standardized treatments. “One cannot say much about the relationship between treatment and symptomatic outcome,” she said. “Treatment may have helped, hurt, done little, or some combination of the three at different times.”
She said the findings have important clinical implications.
“Temperamental symptoms interfere with psychosocial functioning, yet no treatment has been developed to treat them,” she said. “In fact, many psychotherapies end before these symptoms can be addressed. We need to develop therapies to address these troublesome symptoms. This would change the treatment that many borderline patients receive, making their temperamental symptoms as much the focus of therapy as their acute symptoms.”
She is an associate professor of psychology at Harvard Medical School and director of the laboratory for the study of adult development at McLean Hospital in Belmont, Mass.
Joel Paris, M.D., said the study confirmed his own research and that of others showing that patients with BPD are liable to continue to have symptoms of mental illness well after the core symptoms of BPD have resolved.
He cited the Collaborative Longitudinal Personal Disorders Study (CLPS), which was summarized in the October 2005 Journal of Personality Disorders.
“In the CLPS study, we found that people got better over time,” Paris said. “They didn't meet criteria for BPD because they stopped doing the really impulsive things. But they continued to be really unhappy.”
He is a professor and chair of the Department of Psychiatry at McGill University in Montreal and editor in chief of the Canadian Journal of Psychiatry. He is also a past president of the Association for Research in Personality Disorders.
The study was supported by grants from the National Institute of Mental Health.
“The Subsyndromal Phenomenology of Borderline Personality Disorder: A 10-Year Follow-Up Study” is posted at<http://ajp.psychiatryonline.org/> under the June issue. ▪



