States React to Passage of Federal Parity Law
State legislative actions on mental health insurance parity in 2009 focused on strengthening statutes that provide fewer insurance mandates than those approved last year under the landmark federal parity law.
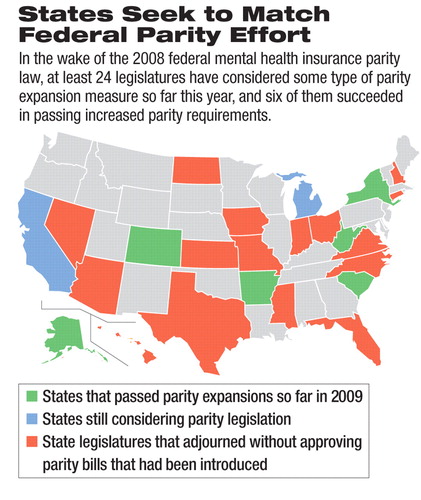
The efforts in some states to conform their statutes to the requirements set by the federal law—the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008—included adding insurance coverage requirements for substance use disorders and making out-of-pocket costs the same as those required for other types of health care. At least 24 legislatures have considered some type of parity expansion measure so far this year, and six have enacted such legislation.
The new state laws—generally aimed at insurance plans not covered under the federal law—aim to simplify state regulators' enforcement efforts, because all plans will have to follow the same rules, according to parity advocates.
The state actions were not required by the federal parity law, because it does not apply to state-regulated insurance plans. Instead, the federal law applies to other insurers, such as those that cover the 82 million people who fall under the Employee Retirement Income Security Act (ERISA). Other plans covered by the federal parity law bring the total number of insured who could be affected by federal parity requirements to about 113 million people.
In Alaska, the legislature updated the state's parity law in April to reflect provisions in the federal parity law, and the governor signed it in August. Had the state not taken action, Alaska Rep. Lindsey Holmes (D) wrote to his colleagues in support of the bill, the state's division of insurance would not have been able to enforce the law when the federal law became effective.
The Alaska bill (HB 222) establishes the same requirements for state-regulated insurers that the federal parity law establishes for plans it regulates. Among the changes is a requirement that state-regulated plans cover the treatment of substance use disorders. The federal law requires parity coverage of treatment for substance abuse only when such coverage is already provided. In addition, the measure matches state law to the Genetic Information Nondiscrimination Act (PL 110-233)—enacted in 2008—barring insurers from discriminating on the basis of subscribers' or applicants' genetic information and requiring continuity of coverage for students taking medically necessary leaves of absence from college.
The other states to pass such measures were New York, Arkansas, Colorado, South Carolina, and West Virginia.
New York voted to make permanent the 2006 parity measure known as Timothy's Law. That law requires insurers issuing group health policies to cover a minimum of 30 inpatient days and 20 outpatient visits for the treatment of mental illness. Other features require health insurance policies of employers with more than 50 employees or members to include care for “biologically based mental illnesses” at the same coverage level as for other medical conditions. These illnesses are defined as “schizophrenia/psychotic disorders, major depression, bipolar disorder, delusional disorders, panic disorder, obsessive-compulsive disorder, bulimia, and anorexia” in adults and children.
“Added to the federal law, [the state insurance parity requirements] are an extremely potent combination,” Seth Stein, J.D., executive director and general counsel of the New York State Psychiatric Association, told Psychiatric News.
Parity legislation in West Virginia (HB 3288) was vetoed by Gov. Joe Manchin III (D) in May over concerns that it would undermine existing state parity law. However, he signed a revised bill in June after the legislature made technical changes. The legislation brings the state's parity law in line with the federal one by prohibiting group health plans that offer mental health and substance abuse coverage from imposing greater treatment limitations and financial requirements on those benefits than on those for other types of medical care.
In Colorado, legislation conforming to the federal parity law was signed on June 1. That legislation (HB 1338), which was sponsored by state Rep. Edward Casso (D), requires coverage of “biologically based mental illness and mental disorders” but does not define them. It also includes provisions to match the federal genetic information discrimination law.
The South Carolina parity measure (SB 390) became law on June 3, without the governor's signature. It expands a 2005 state parity law by adding substance abuse coverage. The expansion was driven by the inclusion of substance abuse coverage in the federal law, said Richard Frierson, M.D., a former president of the South Carolina Psychiatric Association. Legislators were willing to support the measure because the state's research on the inclusion of substance abuse coverage for its employees since 2002 showed minimal additional costs.
In addition, expanded parity coverage could have many important long-term benefits for the state. “This will help increase productivity [of people with a substance use disorder], so in the long run it could save the state a lot of money,” Frierson told Psychiatric News.
The legislation enacted in Arkansas (HB 2195) in April copied federal parity requirements for ERISA plans and applied them to insurers regulated by state law. These new coverage requirements also specifically include insurers that cover state and school employees.
Legislatures in California and Michigan had not finished work for the year at press time and continued to consider enactment of parity expansions.
The Alaska bill is posted at<www.legis.state.ak.us/basis/get_fulltext.asp?session=26&bill=HB222>; South Carolina:<www.scstatehouse.gov/sess118_2009-2010/prever/390_20090514.htm>; Colorado:<www.leg.state.co.us/clics/clics2009a/csl.nsf/fsbillcont3/4B1364ED512F0F01872575890071DD65?open&file=1338_enr.pdf>; West Virginia:<www.legis.state.wv.us/Bill_Status/bills_text.cfm?billdoc=HB3288%20ENR%20SUB%202.htm&yr=2009&sesstype=RS&i=3288>; Arkansas:<www.arkleg.state.ar.us/assembly/2009/R/Bills/HB2195.pdf>.▪



