Prospective Study Questions Beliefs on Prevalence of Mental Illness
A prospective longitudinal study suggests that retrospective surveys, though fairly reliable for short-term snapshots, may be off the mark in estimating lifetime prevalence rates of common mental disorders in the general population.
Large-scale surveys conducted in the community, such as the National Comorbidity Survey (NCS) and NCS-Replication (NCS-R) in the United States and the New Zealand Mental Health Survey (NZMHS), have estimated that one-fourth to one-third of the general population have suffered an anxiety disorder in their lifetime, and 17 percent to 19 percent have had symptoms that met the criteria for major depression. However, a prospective study published online September 1 in Psychological Medicine indicates that about half (49.5 percent) of adults up to age 32 have experienced at least one episode of anxiety disorder, and 41 percent have experienced at least one episode of depression at some point in their lives.
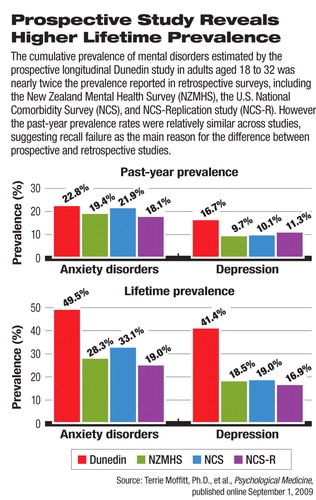
Chart. Prospective Study Reveals Higher Lifetime Prevalence
The study authors, led by Terrie Moffitt, Ph.D., the Knut Schmitt-Nielsen Professor of Psychology and Neuroscience at Duke University, analyzed data from the prospective, longitudinal Dunedin Multidisciplinary Health and Development Study. More than 1,000 people born in Dunedin, New Zealand, from April 1972 through March 1973 were registered at birth to participate in the study and were periodically assessed for health status as they aged.
The participants were assessed for mental disorders at ages 18, 21, 26, and 32 by mental health professionals using DSM-III-R (before 1994) or DSM-IV (after 1994) criteria. The study had an excellent follow-up rate, as 96 percent of the study participants who were alive at the last time point (32 years) were assessed.
The Dunedin study highlights the key divergence between prospective and retrospective epidemiological data on mental illnesses: Prospective, longitudinal data reveal a much higher long-term prevalence than retrospective data that rely on respondents' recall.
Knowing the true prevalence of mental disorders is important for estimating the economic burden, setting public-health policy, allocating resources, and changing public perception and stigma about mental illness, the authors noted.
Retrospective Data Undercounted
Why is there such a large discrepancy between researchers' estimation of cumulative lifetime prevalence? “Recall failure, the fundamental difference between prospective versus retrospective measurement,” the authors wrote, “is the likely explanation.
The explanation is supported by the similarity between the Dunedin study and previous retrospective data in short-term prevalence of mental disorders. The past-year prevalence averaged 23 percent for any anxiety disorder, 17 percent for depression, and 13 percent for alcohol dependence across all assessments during the Dunedin study. These rates approximate the past-year prevalence found in the NCS, NCS-R, and NZMHS, which also implies that the assessment method and validity of the Dunedin study were not significantly different from those of the previous surveys.
That retrospective surveys are vulnerable to recall failure is a known phenomenon in mental health. Previous studies have shown that the proportion of patients who remember they have been diagnosed with depression decreases progressively over time. Moffitt and coauthors cited a body of research that illustrates the unreliability of retrospective mental health epidemiological data, which are largely based on recall of symptoms. For example, among patients who had been hospitalized for depression, half could no longer recall enough symptoms to meet the diagnostic criteria for depression 25 years later to be identified as a lifetime case. Ten percent of people who had been diagnosed with depression could not be identified as lifetime cases in a reinterview after only three years.
Another problem with counting lifetime prevalence of mental disorders was symptom changes over time. Unlike other chronic diseases that persist or progress once diagnosed—such as hypertension or diabetes—common mental disorders often fluctuate in severity and symptoms among some but not all patients. Moffitt and coauthors found that many young adults in the Dunedin cohort did not experience chronic or recurrent disorders, even though their symptoms at one point were severe enough to meet the diagnostic criteria. More than half of those with a lifetime prevalence of anxiety, depression, alcohol dependence, or cannabis dependence were diagnosed with the disorder at only one of the four assessments.
“Epidemiologists agree that prospective studies are more reliable than retrospective studies,” Darrel Regier, M.D., M.P.H., executive director of the American Psychiatric Institute for Research and Education (APIRE) and director of research at APA, told Psychiatric News. To understand what really happens over time, longitudinal studies capture a lot of data that are missed by cross-sectional studies, he noted.
Validity of Diagnostic Criteria Debated
The higher-than-expected cumulative prevalence of mental disorders adds fuel to a long-running argument that diagnostic criteria are too loose and that too many people are unnecessarily diagnosed with mental disorders. A high prevalence by itself, however, does not invalidate a diagnosis. For example, almost every person who has normal blood pressure at 55 will develop hypertension at some point in the rest of his or her life, according to the Framingham Heart Study.
The authors of the Dunedin study believe that their data have probably still underestimated the lifetime prevalence of these mental disorders, because the study cohort was followed only to age 32. They stressed that their findings are “uninformative (and agnostic) about the validity of diagnoses of depression, anxiety, and substance dependence as defined by DSM-IV,” which is “a separate debate.” Meanwhile, the debate about the validity of DSM diagnostic criteria continues within and outside of psychiatry.
Regier, who is the vice chair of the DSM-V task force, hopes the revised diagnostic manual will put some of the controversies to rest.
Regier and William Narrow, M.D., M.P.H., associate director of research at APA and APIRE, both said that the DSM-IV criteria have validity issues inherited from DSM-III, particularly in the community patient sample.
“DSM-III criteria were developed without epidemiological data, and... were based mostly on inpatient data with some outpatient evidence,” said Regier. In other words, these diagnostic criteria worked well in describing patients who are already in psychiatric care. These criteria were necessary and extremely useful at the time to begin to describe and classify mental disorders systematically and build a framework for epidemiological studies. However, in describing the complex presentations of mental disorders outside psychiatric hospitals and epidemiological research, the DSM criteria have encountered difficulties. The criteria are not always helpful in setting appropriate thresholds for those individuals in the community, as captured by this and other epidemiological studies, who apparently meet the criteria but have no need for treatment because of mild severity or a self-limiting episode, Regier and Narrow pointed out.
“The public and media assume that everyone who meets criteria for a DSM diagnosis in a community survey should automatically get treatment, but that is not true,” said Narrow. He gave an example: If a person with a phobia to an object (e.g., snakes) can avoid the object all his life without functional impairment, he may not need treatment for the phobia.
Thus, Regier said, an important goal for DSM-V is to revise the diagnostic criteria substantially, particularly by integrating dimensional severity criteria and symptomatic information across current criteria boundaries, which would make them more useful for clinicians to better identify patients who have underlying psychopathology and to provide a measurement-based approach to treatment.
Rather than expanding the diagnoses of mental disorders as some people fear, the DSM-V task force is aiming to make the diagnoses clearer and more precise and to help epidemiologists set better thresholds for clinically significant mental disorders in community settings, said Regier and Narrow, and these changes will be informative for identifying patients in need of treatment.
An abstract of “How Common Are Common Mental Disorders? Evidence That Lifetime Prevalence Rates Are Doubled by Prospective Versus Retrospective Ascertainment” is posted at<journals.cambridge.org/action/displayAbstract?fromPage=online&aid=6121524&fulltextType=RA&fileId=S0033291709991036>.▪



