Web Tool Hoped to Strengthen Doctor-Patient Bond
Abstract
The therapeutic alliance is a hallmark of mental health care. Now the Substance Abuse and Mental Health Services Administration (SAMHSA) follows an emerging trend to give both sides of that alliance a better way to decide among treatment options.
SAMHSA has introduced an online site promoting shared decision making about choices in antipsychotic medication among patients and clinicians.
Shared decision making is a way “to help balance clinical information about mental health conditions and treatment options with an individual’s preferences, goals, and cultural values and beliefs,” according to the Web site, which SAMHSA calls a “tool.” It is intended as the first step in a proposed series of such decision tools for other psychiatric disorders, said Paolo Del Vecchio, M.S.W., acting director of the Center for Mental Health Services at SAMHSA.
“We hope the tool improves communication and the therapeutic relationship between providers and the people receiving treatment,” Del Vecchio told Psychiatric News. “We see it as an innovative use of technology to produce the benefits that shared decision making brings.”
“I’m glad the mental health community is going to take on shared decision making,” said Jessie Gruman, Ph.D., president of the Center for Advancing Health in Washington, D.C., which advocates for increased engagement by individuals in their health and health care. “This represents a seismic shift in the patient-clinician relationship. It challenges clinicians’ traditional thinking about their role. For patients, it is equally daunting because it demands courage to engage in a new way with their clinician.”
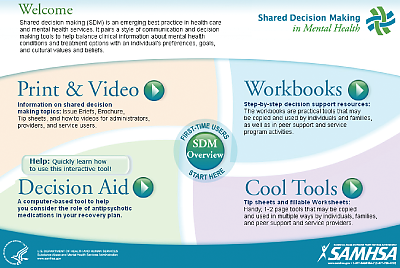
Opening the Web site reveals five links, marked Print & Video, Decision Aid, Workbooks, Cool Tools, and SDM Overview. The last link serves as an introduction to the other four options. Each section contain a mix of resources, some aimed at patients, some for clinicians, some for families. A tutorial can assist viewers to navigate through the Web site.
The impetus for the program grew out of experience with other health conditions, particularly breast cancer, showing that using decision aids for patient involvement in their own care positively affected treatment outcomes, said Del Vecchio. The project took three years from inception to release.
Vignettes in the videos of patients talking through treatment decisions with practitioners were scripted but are portrayed by actual patients and clinicians, he said.
Gruman has her reservations about the new SAMHSA site but also sees its potential for benefiting patients.
“It’s condescending (‘cool’) and jargony (‘tools’) at the same time,” she said in an interview. “Could people with schizophrenia find their way through it?”
Many of the suggestions and examples, while well-intended, could be intimidating to patients, said Gruman, author of The Experience of the American Patient: Risk, Trust, and Choice (Health Behavior Media, 2009). Patients may feel they’re taking a risk by moving to change the relationship, as the shared decision making ideal suggests.
The tool was field tested before release on groups of patients and clinicians, said Del Vecchio.
However, SAMHSA’s influence in the clinical community might move more clinicians to place some of the printable material in offices and waiting rooms.
“That signal would be one of the most important invitations a clinician can make to the client,” said Gruman. “The information is useful, but the presence of the tool will tell the patient that the clinician is giving permission to alter the relationship between the two.”
The tool represents just a beginning, said Del Vecchio. “Our next steps will be to continue to encourage its use by consumers and providers even as we update the material,” said Del Vecchio. “We intend to expand to include other conditions, beginning with medical treatment of addictions, primarily opiate addiction.”
“Shared Decision Making in Mental Health” can be accessed at www.samhsa.gov/consumersurvivor/sdm/StartHere.html.



