High Opioid Use by Veterans Raises Serious Concerns
Abstract
Veterans of the wars in Iraq and Afghanistan diagnosed with mental health disorders are about twice as likely to be prescribed opioid pain medications and to have worse clinical outcomes than similar veterans without such diagnoses, according to a study in the March 7 Journal of the American Medical Association.
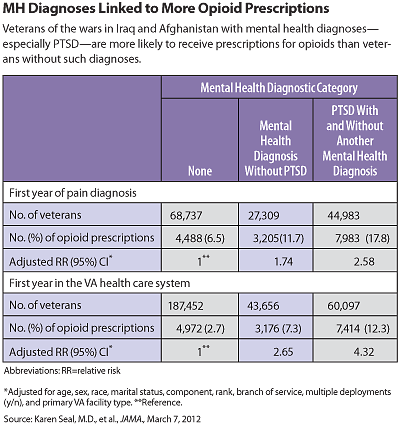
The retrospective cohort study of 141,029 veterans treated for noncancer pain between 2005 and 2008 found that 6.5 percent with no mental health diagnosis were prescribed opioids, compared with 11.7 percent of those with a mental health diagnosis but not posttraumatic stress disorder (PTSD) and 17.8 percent with PTSD.
The veterans with PTSD were more likely to receive higher doses of opioids, more than one opioid, and to refill prescriptions a week earlier than patients without PTSD. They were also at significantly increased risk for depression, anxiety, alcohol or drug use disorder, and traumatic brain injury.
“These findings support further efforts to improve care of patients with comorbid pain and PTSD because of the heightened risk of self-medication with opioids and substance abuse in veterans with PTSD,” wrote lead author Karen Seal, M.D., M.P.H., of the University of San Francisco, and colleagues. “These patients may benefit from biopsychosocial models of pain care including evidence-based nonpharmacologic therapies and nonopioid analgesics.”
“Patients with PTSD often present with somatic complaints and pain,” said U.S. Army Col. David Benedek, MC, a professor and deputy chair of the Department of Psychiatry and associate director of the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences in Bethesda, Md. He was not involved with Seal’s research.
“They may well receive opioid analgesics from sources such as their primary care physicians for these complaints,” said Benedek in an interview. “Patients with PTSD may seek to self-medicate with narcotics, which may contribute to the early requests for refills.”
The common adverse clinical outcomes associated with opioid use in these patients included injuries or accidents, overdoses, self-inflicted injuries, and violence-related injuries, said the researchers.
Risk for such adverse outcomes was greatest for patients with PTSD, compared with vets without a mental health diagnosis, or to those with a mental health diagnosis other than PTSD.
Many veterans with psychiatric problems seek care in VA primary care settings to minimize stigma, wrote Seal. “As in the broader community, most VA primary care clinicians lack specialized training in the management of comorbid pain and PTSD.”
In fact, the frequent prescription of opioids for patients with substance use disorders raised concerns for the authors, even though VA guidelines suggest heightened awareness about the use of opioids in those cases.
It was not clear if the authors controlled for degree of injury, said Benedek. “It may well be that veterans with PTSD in this study had more severe injuries than others with pain diagnoses not related to combat, and therefore required more pain medication,” he said.
Seal and colleagues suggest caution in the future when treating veterans with comorbid physical and psychological pain. “Integrated treatments that target both mental health disorders and pain simultaneously are effective for both problems and may decrease harms resulting from opioid therapy,” they noted.
Finally, extensive use of opioid analgesics is a national concern and not one limited to veterans, Benedek emphasized.
“Use of these medications for chronic back or knee pain, for example, is also an issue, since many soldiers are also experiencing chronic muscle and arthritic symptoms due to the excessive loads they were carrying while deployed,” he said. “So we must keep in mind that PTSD may be part of this issue, but excessive physical demands and treatment for joint-pain discomfort in primary care may be another and perhaps accounts for most of the use of these medications among veterans.”
The study was funded by the Department of Veterans Affairs Health Services Research and Development program and the National Heart, Lung, and Blood Institute. 
“Association of Mental Health Disorders With Prescription Opioids and High-Risk Opioid Use in U.S. Veterans of Iraq and Afghanistan” is posted at http://jama.ama-assn.org/content/307/9/940.abstract.



