Schizotypal Personality Disorder Linked to Brain Changes
Abstract
Men with schizotypal personality disorder have reduced gray matter in a number of brain areas, and this paucity may be responsible for their negative symptoms.
Men with schizotypal personality disorder have reduced brain matter in a number of areas.
This finding was reported by Robert McCarley, M.D., chair of psychiatry at Harvard Medical School, and his colleagues online February 6 in JAMA Psychiatry.
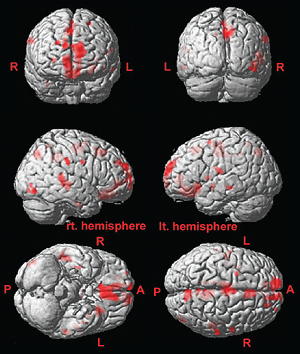
These brain images are taken from subjects with schizotypal personality disorder. The gray matter deficits linked with the negative symptom of social isolation are in red.
The researchers launched their study by placing the following ad in the community: “A study at Harvard Medical School seeks right-handed people who believe they have ESP, telepathy, or a ‘sixth sense’; often mistake noises for voices; sense the presence of others when alone; have extreme social anxiety (or discomfort) in social situations involving unfamiliar people; and have few friends.”
The ad used DSM-IV diagnostic criteria for schizotypal personality disorder, which include odd beliefs and superstitions or a “sixth sense,” abnormal perceptual experiences, odd thinking and speech, suspiciousness, constricted affect, peculiar appearance or behavior, no close friends, and extreme social anxiety.
Some 3,000 people responded to the ad, of whom some 1,500 were then interviewed by phone. Fifty-four were ultimately diagnosed with schizotypal personality disorder and enrolled in the study.
After that, McCarley and colleagues placed another ad to find 54 control subjects who were matched with the first group on age, handedness, and IQ score.
They then used magnetic resonance imaging (MRI) to visualize the brains of all 108 subjects.
The schizotypal personality subjects had significantly less gray matter in widespread temporal, frontal, and parietal regions of the brain than did controls. Generally the deficits were the same as those known to exist in patients with schizophrenia, but less severe. While he and his colleagues had anticipated such a finding, they didn’t expect it to be so “striking,” McCarley said in an interview with Psychiatric News.
The researchers also looked to see whether gray matter deficits in the schizotypal subjects could be significantly linked to their negative symptoms. It turned out that they could. For example, social isolation was linked to 18 regions with gray matter deficits, introversion to 13 such regions, and restricted emotions to 11 such regions. Some of the gray matter deficits linked to negative symptoms in schizotypal personality disorder subjects have also been associated with negative symptoms in subjects with schizophrenia, McCarley said.
Thus it looks as if reductions in gray matter may contribute to the negative symptoms of schizotypal personality disorder, just as they may contribute to those symptoms in schizophrenia, the researchers believe.
And if a paucity of gray matter in various regions of the brain is at least partially responsible for the negative symptoms of schizotypal personality disorder, then the findings have clinical implications, McCarley said.
“Our current study showed relationships between negative symptoms and local gray matter volume reductions, including medial frontal regions…and the superior temporal gyrus (the sensory auditory cortex). There is now beginning evidence in schizophrenia that computerized cognitive and social training can act on and improve function of both these regions…There are, thus, possibilities that cognitive training could change functions and/or volumes of the…regions found to be volume-reduced in our study and thereby improve negative symptoms in subjects with schizotypal personality disorder and hence their quality of life.”
Curiously the researchers were not able to find in their schizotypal subjects any link between gray matter reductions and positive symptoms such as magical thinking and illusions. Therefore “we need to clarify pathology for positive symptoms in subjects with schizotypal personality disorder and relate [such pathology] to volume reduction and other biological measures,” McCarley said.
He and his colleagues are already making inroads in unmasking the biological basis of positive symptoms, he noted. They are using magnetic resonance spectroscopy to measure two neurotransmitters—GABA and glutamate—in the left superior temporal gyrus in schizotypal personality subjects. “Early initial data indicate lower GABA and higher glutamate metabolites are associated with more positive symptoms. We are excited by these initial findings and are applying for a grant for a more extensive study.”
The study was funded by the National Institute of Mental Health, Department of Veterans Affairs, and National Health and Medical Research Council of Australia. ■
“Globally and Locally Reduced MRI Gray Matter Volumes in Neuroleptic-Naive Men With Schizotypal Personality Disorder” is posted at http://archpsyc.jamanetwork.com/article.aspx?articleid=1568958.



