Increase in Off-Label Antipsychotic Use Seen in Canadian Youth
Abstract
Researchers sound an alarm on the “exponential rise” in antipsychotic prescriptions for children and adolescents and urge closer monitoring of prescribing practices.
The number of children and adolescents aged 18 and younger who were prescribed a second-generation antipsychotic (SGA) increased by 18 times from 1996 to 2010 in British Columbia, according to findings published in the June Canadian Journal of Psychiatry.
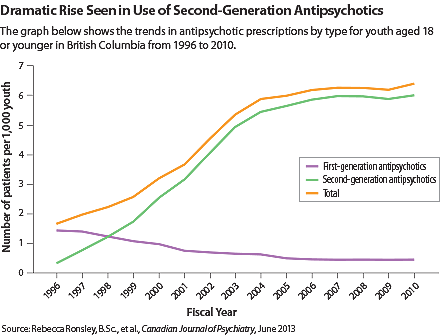
The authors collected prescription information from the province’s health registry on all outpatient data, which also links most prescriptions to diagnoses and to the types of physicians who wrote the prescriptions. They found that 0.33 youth per 1,000 received an SGA prescription in Canada’s 1996 fiscal year (April 1, 1996 to March 31, 1997), while 5.98 youth per 1,000 did so in the 2010 fiscal year.
A very different trend characterized use of first-generation antipsychotics, which dropped from 1.43 per 1,000 youth in 1996 to 0.46 per 1,000 in 2010. Overall, the number of youth receiving antipsychotics increased nearly fourfold from 1.66 per 1,000 to 6.37 per 1,000 (see graph).
The rise was primarily driven by prescription increases in both male and female adolescents aged 13 to 18 and in boys aged 6 to 12, with the average numbers of patients receiving antipsychotic prescriptions up by 3.7 to 4.4 times. Antipsychotic prescriptions for girls aged 12 and younger and boys aged 5 and younger remained relatively flat.
In 2010, the most common diagnoses linked to pediatric antipsychotic prescriptions were depressive disorders, hyperkinetic syndrome of childhood (including attention-deficit/hyperactivity disorder [ADHD]), and neurotic disorders (including anxiety, dissociative, phobic, and obsessive-compulsive disorders). Antipsychotics have not been approved by Health Canada for most of these indications in children, the authors stated.
Psychiatrists were the largest category of physicians to write an antipsychotic prescription for children and adolescents, accounting for 38.6 percent of first-time antipsychotic prescriptions in 2010, followed by general practitioners, who prescribed 34.3 percent. Pediatricians prescribed 15.6 percent of the antipsychotics for this population.
Efforts should be made to “disseminate the results of this and other epidemiologic research about the high prevalence of metabolic complications of SGAs to key stakeholders, specifically the highest prescribers in children and youth: psychiatrists, family physicians, and pediatricians,” Constadina Panagiotopolous, M.D., the study’s senior author, told Psychiatric News. “We have been funded to develop an online interactive module…as an educational resource for evidence-based prescribing as well as to raise awareness of recently published Canadian guidelines for monitoring and management of metabolic complications in children and youth prescribed SGAs.”
Panagiotopoulos is an associate professor of pediatrics at the University of British Columbia and an endocrinologist at British Columbia Children’s Hospital.
“When antipsychotics are prescribed for children, there is always a concern about balancing the benefits and the risks, such as weight increase, metabolic syndrome, diabetes, and tardive dyskinesia,” Louis Kraus, M.D., a professor of child and adolescent psychiatry at Rush University Medical Center in Chicago and chair of APA’s Council on Children, Adolescents, and Their Families, commented to Psychiatric News. “The rise in SGA prescriptions in pediatric patients parallels the trend in adult patients during the same period.”
Kraus pointed out that the Canadian study included 18-year-olds in the analysis, a group that is considered adults in the United States. Most of the antipsychotic drugs have been approved in the United States as adjunct treatment for refractory depression in adults. He also noted that there is clinical and research evidence to support the efficacy of antipsychotics to treat refractory depression, tic disorder, severe behavioral symptoms, and mood disorders with psychotic features in younger patients. Some SGAs have been approved in the United States to treat behavioral symptoms in children with autism.
“The reality is that many medications we use are off label, but it doesn’t mean we shouldn’t use them,” Kraus said. The AMA supports clinical decisions to use medications off label to help patients, as long as the risks and benefits are carefully considered, and patients or their guardians understand that the medication is used off-label.”
“In these patients [who may benefit from antipsychotics], the clinical presentation is often complicated,” Kraus noted. “We have to be very conservative in using antipsychotics for children.” Considering that data show many of these prescriptions were written by nonpsychiatrists, “I strongly recommend that family physicians and pediatricians consider getting a consultation with a child and adolescent psychiatrist to review the diagnosis and obtain appropriate informed consent with the patient and/or guardian before prescribing antipsychotics for children,” he urged.
The study was funded by the British Columbia Mental Health and Addiction Services and the Child and Family Research Institute, a network of medical and research institutions in Western Canada. ■
An abstract of “A Population-Based Study of Antipsychotic Prescription Trends in Children and Adolescents in British Columbia, From 1996 to 2011” is posted at http://publications.cpa-apc.org/browse/documents/598.



