Clinicians in DSM-5 Field Trials Have Positive Response to Revisions
Abstract
Patient-rated symptom measures will be useful in measurement-based care, which is being incorporated in emerging integrated-care systems.
DSM-5 was found to be clinically useful and easy to use by clinicians in routine clinical practice, according to results from the second arm of field trials testing the new manual, which was published in May.
Importantly, patients in the field trials also said that the “cross-cutting symptom measures”—a tool for patients to report their own evaluation of their symptoms—would help their clinicians better understand their symptoms. That’s crucial because these new measures, which appear in Section III of the manual, can serve as a baseline for measurement-based care, a quality indicator that is being incorporated in integrated-care networks and electronic health record systems.
The results of this arm of field trials were published online July 15 in Psychiatric Services.
The first arm of field trials, reported last November in the American Journal of Psychiatry, tested the reliability of the new diagnostic criteria—that is, the likelihood that diverse clinicians would apply the same diagnosis to the same patient—at high-volume academic centers. The second set of field trials was designed to assess the clinical utility and feasibility of the diagnostic criteria as tested by a range of mental health clinicians in routine clinical practice and the cross-cutting symptom measures as assessed by patients recruited from the clinicians’ active caseloads. “The Routine Clinical Practice (RCP) Field Trials suggest that the DSM-5 approach is feasible and clinically useful in routine care settings and acceptable to both clinicians and their patients,” said the authors of the report. They include Darrel Regier, M.D., M.P.H., director of APA’s Division of Research; William Narrow, M.D., research director of the DSM-5 Task Force; and staff of the Division of Research. The principal investigator for the field trial was Eve Mościcki, Sc.D., M.P.H.
The field trials were conducted in a wide range of practice settings in the United States, Canada, Australia, and the United Kingdom. Data collection took place over a six-month period from fall 2011 through early 2012. Clinicians were recruited from two groups: a random sample of 9,460 psychiatrists drawn from the AMA Physician Masterfile and a volunteer sample of more than 5,600 mental health clinicians, recruited primarily on the DSM-5 Web site (http://www.dsm5.org).
Participants were required to complete extensive training on the Internet-based reporting system used for the trial, as well as training for acquiring consent from enrolled patients while also acquainting themselves with the DSM-5 criteria.
“It was a time-intensive process,” Mościcki told Psychiatric News, “but those who did so from all disciplines and from both the U.S. and international sites found this to be a rewarding experience. The total number of clinicians involved in this field trial alone is far higher than were involved with the previous DSM field trials.”
The final sample of 621 participants included 154 psychiatrists, 77 licensed doctoral-level clinical psychologists, 111 clinical social workers, 33 advanced practice psychiatric/mental health nurses, 126 licensed counselors, 113 licensed marriage and family therapists, and seven licensed master’s-level psychologists. Each clinician was asked to report on at least one patient randomly sampled from his or her active caseload; a total of 1,269 adult and child patients were enrolled.
Patients or their proxies completed the patient measures and a brief set of questions about their impression of the measures before meeting with the clinician. The results and interpretation of the patient-reported measures were transmitted to a database for clinician review before patient evaluation.
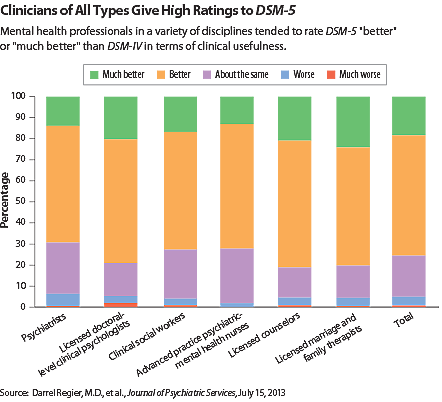
The study results showed that large proportions of clinicians reported that the DSM-5 approach was very or extremely easy to apply for assessment of both pediatric (51 percent) and adult (46 percent) patients and very or extremely useful in routine clinical practice for pediatric (48 percent) and adult (46 percent) patients. Similar patterns in evaluations of feasibility and clinical utility were observed among clinicians from various disciplines (see chart).
Overall, clinicians considered the DSM-5 approach to diagnosis to be better (57 percent) or much better (18 percent) than that of DSM-IV. Of the clinicians with pediatric patients, more than 75 percent reported that the DSM-5 approach for all disorders was better or much better than that of DSM-IV. Nearly 85 percent of those treating patients with attention-deficit/hyperactivity disorder (ADHD) rated the approach to ADHD better or much better.
Similarly, approximately 75 percent of the clinicians with adult patients reported that the DSM-5 approach for all disorders was better or much better than that of DSM-IV for assessment of adult patients. The most favorable ratings were reported for diagnoses of posttraumatic stress disorder, personality disorders, bipolar II disorder, substance use disorders, and somatic symptom disorder.
“These were among the most significantly revised disorders in DSM-5, yet the revised criteria received some of the highest ratings for their feasibility and clinical utility,” Regier and colleagues said. “This finding suggests that DSM-5 criteria will facilitate better care for patients who suffer from these disorders.”
Patients, including children aged 11 to 17 (47 percent), parents of children aged 6 to 10 (64 percent), parents of adolescents aged 11 to 17 (72 percent), and adult patients (52 percent) reported that the cross-cutting measures would help their clinicians better understand their symptoms.
The researchers said that these measures will not only inform clinical assessment, but can be the basis for quality-improvement measures that are being mandated for use in electronic health record systems. “In clinical practice, a mental disorder diagnosis is only one aspect of a clinical formulation that also includes the presenting complaint; past medical history; a mental status examination; a review of physical and mental systems; and an assessment of the patient’s family, social, and cultural context, ability to perform various life activities, environmental exposures, and other risk factors,” they noted. “A diagnosis made in this context can benefit from the type of patient-generated information introduced in DSM-5—which is supported by the levels of patient approval reported here—and will become increasingly standardized as part of federally mandated ‘meaningful use criteria’ for electronic health records.” ■
“Testing DSM-5 in Routine Clinical Practice Settings: Feasibility and Clinical Utility” is posted at http://ps.psychiatryonline.org/journal.aspx?journalid=18.



