Changes Needed in Mental Health Care of Children, Experts Agree
Abstract
Hospital administrators, pediatricians, psychiatrists, advocacy groups, and legislators share strategies for broadly improving mental health care for America’s children and adolescents.
Overcoming the barriers and providing better mental health care for children will require a wide range of changes, from public policies to clinical practices and from local hospitals and school districts to federal laws and regulations. The need to change the current way youth are treated for mental health problems was the key message arising from a multidisciplinary summit held in Washington, D.C.
The summit was organized by Children’s National Medical Center, one of the largest children’s hospitals in the country. The summit, titled Children’s National Summit on Improving Children’s Mental Health Care, took place on May 7 and was attended by administrators of children’s hospitals, directors of pediatric or psychiatric departments, medical association leadersh, state and federal health care regulators, and several members of Congress.
The summit was a response to a 2013 call to action by the White House to effect improvements in childhood mental health care, according to Kurt Newman, M.D., president and CEO of Children’s National Medical Center. The call to action was in part spurred by tragic incidents such as the Sandy Hook Elementary School shooting in Newtown, Conn.

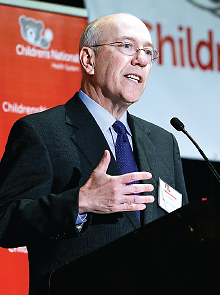
Patrick Kennedy, a former member of Congress and now a senior advisor to APA, gives the keynote speech at a summit on child mental health care last month at Children’s National Medical Center. “We are operating in a ‘fail-first model’ ” with regard to children, he said.
Patrick Kennedy, a former member of Congress and now a senior advisor to APA, gave the keynote speech. He discussed his personal struggle with bipolar disorder and addictions, noting that there is inadequate screening and intervention for early mental and behavioral disorders in primary care settings. “We are operating in a ‘fail-first model,’ ” he said, as he compared patients’ access to mental health care with treating patients with diabetes only when their illness is so severe that they require amputation of a limb.
During his tenure in Congress, Kennedy was the lead sponsor of the Mental Health Parity and Addiction Equity Act, which passed in 2008. In his speech, Kennedy railed against what he saw as lagging accountability for and enforcement of the implementation of the mental health parity law. He partially blamed the stigma against mental illness for the resistance among government officials and lawmakers to enforcing parity reimbursement and coverage by private insurance companies, which has allowed some insurance plans to continue to underfund mental health care. Other attendees at the summit, including children’s hospital administrators from across the country, also cited inadequate funding and reimbursements as major barriers to implementing and expanding mental health services that have been proven to be beneficial for patients, families, and communities.
The lack of financial incentives is one contributing factor to the shortage of qualified mental health professionals to meet the overwhelming needs from children and families. In addition to the lack of funding, “we don’t have the specialists, especially for child and adolescent mental health, to provide the services needed,” Virginia’s Secretary of Health and Human Services, William Hazel, M.D., acknowledged.
Kurt Newman, M.D., CEO of Children’s National Medical Center, says the center’s mental health summit is a response to the 2013 call to action by President Obama to improve childhood mental health.
Pediatricians and primary care physicians need better education and training to assume responsibility for screening and treating mental illness at an early age, Newman commented.
Paramjit Joshi, M.D., the president of the American Academy of Child and Adolescent Psychiatry, emphasized the critical importance of early identification and prevention, because half of all the serious psychiatric disorders occur by age 14, and three-quarters by age 24. Early intervention can significantly reduce long-term severity and disability, she said. Joshi is director of psychiatry and psychology programs at Children’s National Medical Center and a member of the Psychiatric News Editorial Advisory Board.
Several speakers emphasized that the fragmentation of mental health screening and treatment services is another major barrier. The need is great for more community-based, integrated mental health collaborations between hospitals and clinics with families and schools, they pointed out.
Sen. Chris Murphy (D-Conn.) discussed the challenge of “rampant criminalization of youths with mental illness” in his state. And Hazel noted a similar burden of caring for youth with mental illness in the Virginia juvenile-justice system. The sad reality, they pointed out, is that prison is often the first or only place many young people with psychiatric disorders can access treatment.
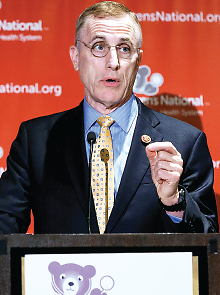
Rep. Tim Murphy (R-Pa.) discusses policies and regulations that raise barriers to providing mental health care for children and adolescents.
Rep. Tim Murphy (R-Pa.), who is also a clinical psychologist, outlined several policies and regulations that hinder mental health care for children and adolescents. In December 2013, he introduced a bill in the House, the Helping Families in Mental Health Crisis Act, which proposes to increase the flexibility in current privacy rules for families and physicians of youth with mental illness to facilitate integrated care. The bill also calls for adding an assistant secretary position to the Department of Health and Human Services, as a way to ensure that federal dollars are spent on effective, evidence-based models of treatment and program effectiveness (Psychiatric News, May 2).
“I’m very optimistic that once we develop a critical mass of awareness of pediatric mental health issues, we will make positive changes on all levels,” Newman told Psychiatric News after the summit. “This summit could play a role in sparking the exchange [of ideas] among mental health and pediatric providers, academics, government agencies, legislators, and advocates . . . [and could] stimulate conversation and open people’s minds.”
Having this summit in Washington, D.C., and bringing together the mental health community and federal and local legislators can also promote political advocacy and promote broad policy reforms that will have greater impact on mental health care, Newman suggested. ■
The text of Murphy’s bill, HR 3717, can be accessed here.



