Health Coaching Effective for Obesity in Severe Mental Illness
Abstract
Having a health-promotion coach is associated with greatly increased fitness-club attendance, which in turn was linked with greater weight loss and improved cardiac fitness in those with serious mental illness.
A health-coaching intervention for obesity appears to be effective in achieving and sustaining clinically significant reductions in cardiovascular risk for overweight and obese individuals with serious mental illness.
That’s the finding of a replication trial of the In SHAPE program, the results of which were published December 12, 2014, in AJP in Advance.
The report is “the first replication study confirming the effectiveness of a health-coaching intervention in achieving clinically significant reductions in cardiovascular risk for overweight and obese persons with serious mental illness and the first study to demonstrate persistent reduction in cardiovascular risk after the active intervention has been withdrawn,” said lead author Stephen Bartels, M.D., of the Department of Psychiatry and the Dartmouth Institute for Health Policy and Clinical Practice at the Geisel School of Medicine at Dartmouth and colleagues.
In SHAPE is a 12-month program consisting of individual weekly meetings in the community with a health-promotion coach, a fitness-club (YMCA) membership, and nutrition education adapted for people with serious mental illness that was found in a previous study to contribute to clinically significant reduction in cardiovascular risk in overweight or obese adults with serious mental illness.
In the new study, Bartels and colleagues randomly assigned 210 individuals with serious mental illness and a body-mass index greater than 25 receiving services in one of three community mental health organizations either to the 12-month In SHAPE program or to fitness-club membership alone. The primary outcome measures were weight and cardiorespiratory fitness (as measured with the six-minute walk test) assessed at baseline and at three-month intervals for 18 months.
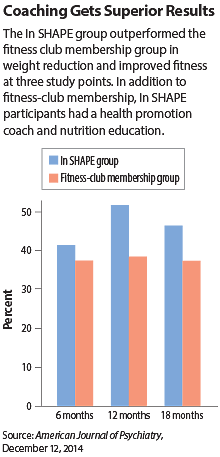
At 12 months, the In SHAPE group had greater reduction in weight and improved fitness compared with the fitness-club membership group. Primary outcomes were maintained at 18 months (see chart). Approximately half of the In SHAPE group achieved clinically significant cardiovascular risk reduction, defined by a weight loss greater than 5 percent or an increase of greater than 50 meters on the six-minute walk test.
“By comparing In SHAPE to an active comparison condition (a fitness-club membership), we were able to test the specific contribution of having a health-promotion coach,” the researchers stated. “Having a health-promotion coach was associated with more than two-and-a-half times the mean amount of fitness-club attendance, which in turn was associated with greater weight loss and improved fitness.”
They added that current efforts to increase life expectancy for people with serious mental illness are focused on improving the quality and delivery of primary health care by integrating “health homes” within mental health care. “These initiatives address the inadequate access to and poor quality of health care experienced by persons with mental illness,” they said. “However, only 10 percent to 15 percent of preventable mortality is estimated to be due to health care access and quality factors, in contrast to health behaviors, which are estimated to account for the majority (57 percent) of a population’s health status and 40 percent of early deaths. By also providing health promotion as a core service, it may be possible to further reduce early mortality while improving both the psychological and physical wellness of the whole person.” ■
“Pragmatic Replication Trial of Health Promotion Coaching for Obesity in Serious Mental Illness and Maintenance of Outcomes” can be accessed here.



