FDA Approves First Treatment for Sexual Desire Disorder in Women
Abstract
The medication will feature a boxed warning to highlight the risk of severe hypotension and loss of consciousness in patients who drink alcohol with the medication and in those who use moderate to strong CYP3A4 inhibitors.
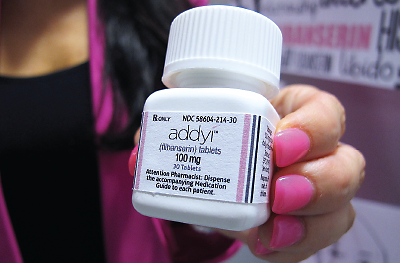
The Food and Drug Administration (FDA) last month approved Addyi (flibanserin) to treat acquired, generalized hypoactive sexual desire disorder (HSDD) in premenopausal women. The medication is the first FDA-approved treatment for sexual desire disorders in men or women.
“The problems associated with low sexual desire are commonly seen in psychiatric practice and may be comorbid with many psychiatric disorders, especially anxiety and mood disorders,” said Robert Segraves, Ph.D., M.S., a professor emeritus of psychiatry at Case Western Reserve University and a member of the Sexual and Gender Identity Disorders Work Group for DSM-III, DSM-IV, and DSM-5. “For the first time, an approved medication can be prescribed for this disorder,” he told Psychiatric News.
Addyi—a serotonin 1A receptor agonist and serotonin 2A receptor antagonist—was rejected twice by the FDA in the past five years after the agency concluded the drug was ineffective and carried too high a risk for side effects. After the setbacks, Sprout Pharmaceuticals, manufacturers of Addyi, along with multiple women’s activist groups launched a campaign against the FDA for being discriminatory toward sexual health products for women that led to a petition of more than 60,000 signatures. After a third submission of data supporting Addyi’s effectiveness, the drug was approved.
Addyi’s effectiveness was evaluated in three 24-week randomized, double-blind, placebo-controlled trials in approximately 2,400 premenopausal women with acquired, generalized HSDD. The average age of the trial participants was 36 years, with an average duration of HSDD of approximately five years. The participants took either an oral 100 mg dose of Addyi or placebo at bedtime.
Across the three trials, women taking Addyi were 10 percent more likely to report at follow-up meaningful improvements in past-month sexual event satisfaction or sexual desire than women being treated with placebo. On average, treatment with Addyi increased the number of satisfying sexual events by 0.5 to 1 additional event per month over placebo. The most common adverse reactions associated with the use of Addyi included dizziness, somnolence, and dry mouth. The mechanism by which Addyi improves sexual desire is currently unknown.
The FDA approved Addyi with a boxed warning to highlight the risk of severe hypotension and loss of consciousness (syncope) in patients who drink alcohol during treatment with Addyi and in those who use moderate to strong CYP3A4 inhibitors that interfere with the breakdown of the medication. The newly approved drug is also contraindicated for those with liver disease.
Because of the increased risk of severe hypotension and syncope due to the interaction between Addyi and alcohol, the FDA is requiring all prescribers of Addyi to enroll and complete training in a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use. Certified prescribers must counsel patients using a Patient-Provider Agreement Form about the increased risk of severe hypotension and syncope and about the importance of not drinking alcohol during treatment with Addyi. Only REMS-certified pharmacies will be allowed to dispense Addyi from a certified prescriber.
Segraves told Psychiatric News that he is hopeful that the approval of Addyi will lead to a renewed interest in human sexuality among psychiatrists and clinical psychologists, and spur more research into ways that low sexual desire can be treated.
The tentative marketing release date for Addyi is October 17, according to Sprout Pharmaceuticals. ■



