Senators Urged to Break Cycle of Jailing People With Mental Illness
Abstract
Using America’s jails to house and provide treatment to people with mental illness wastes lives and taxpayers’ money, senators are told.
Senators gathered on Capitol Hill in February to hear testimony and voice their opinions on several bills aimed at “breaking the criminal justice/mental health connection,” in the words of Judiciary Committee Chair Sen. Charles Grassley (R-Iowa).

“One of the worst things we can do is stigmatize people with mental illness,” Sen. Al Franken (D-Minn.) tells those at a hearing on breaking the cycle between the mental health and criminal justice systems.
The overrepresentation of people with mental illness in American jails and prisons and the consequent rise in costs to state and local governments have pushed lawmakers to action in recent years.
“We won’t fix this problem by reducing it to sound bites or silos,” said Grassley. He reiterated his support for multifaceted legislation expanding training for law enforcement officers, strengthening the background check system for gun purchases, directing federal judges to use mental health courts, and addressing co-occurring substance use disorders in prisoners.
“I am heartened that this issue is getting attention from both sides of the aisle and both sides of the Capitol,” responded Sen. Al Franken (D-Minn.). “Using the criminal justice system as a substitute for a functioning mental health system doesn’t make sense for law enforcement, for the courts, for individuals, or for taxpayers.”
Franken is a cosponsor with Sen. John Cornyn (R-Texas) of the Comprehensive Justice and Mental Health Act (CJMHA), which reauthorizes the existing Mentally Ill Offender and Crime Reduction Act and was passed by a voice vote in the Senate in December 2015. Another bill introduced by Cornyn would expand police crisis-intervention teams (CIT) and treatment-based alternatives to incarceration and improve post-release options for former prisoners, among other provisions.
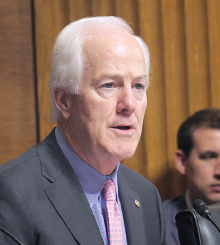
Sen. John Cornyn (R-Texas) says that he hopes the hearing will raise public awareness about mentally ill people in the criminal justice system and apply pressure to find a solution.
“The current system of warehousing people with mental illness is not working,” agreed Cornyn. “Screening people coming into the criminal justice system for mental illness and diverting them helps break the cycle.”
One witness at the hearing, Sheriff Susan Pamerleau of Bexar County, Texas, noted that 60 percent of the people in her jail had a mental illness, making the jail the county’s largest mental health provider, and a costly one.
“The average cost per day of a prisoner is $60 to $65, but in the mental health unit, it’s $200 to $250 a day,” said Pamerleau. Since 2009, she said, CIT training has been mandated for all patrol officers, who can now screen subjects before arrest and take them to a mental health clinic, if necessary. Use of force has declined, and the county has saved $15 million in officer costs.
“The federal government spends $2 billion on local law enforcement but only 1 percent of that involves mental illness,” said Cornyn. Cost-shifting could be a problem, so funding needs to be viewed more comprehensively, he said.
“It’s important to appropriate money in order to save money,” said Franken. “We need more beds in the mental health system to avoid sending people to jail.”
Psychiatrist Fred Osher, M.D., told the panel that the annual entry of two million people into America’s jails and prisons was a “growing national tragedy.”

From left: Author Pete Early, psychiatrist Fred Osher, M.D., and Bexar County, Texas, Sheriff Susan Pamerleau called for improving the mental health system to divert more people with mental illness from county jails.
States and localities face major obstacles in addressing the problem, said Osher, director of Health Systems and Services Policy for the Council of State Governments Justice Center. “These include inadequate data to inform policy changes, operating with minimal resources, and needing better coordination between criminal justice, mental health, substance use, and other agencies.”
Osher, too, backed alternatives to jail when people are in crisis; more CIT training for police; greater use of drug, veteran, and mental health courts; and better connection to community treatment and supervision following release.
The Council of State Governments Justice Center is working with the National Association of Counties and the American Psychiatric Association Foundation on the Stepping Up initiative to reduce the numbers of people with mental illness and co-occurring substance use disorders in jails. As part of this initiative, the organizations are sponsoring the Stepping Up National Summit from April 17 to 19 in Washington, D.C., during which teams from 50 U.S. counties will participate. Each team will include at least one county commissioner or supervisor, a jail administrator, and a county behavioral health administrator. Others, like judges, prosecutors, advocates, and people with a mental illness, may be included as well.
Bills in addition to those of Franken and Cornyn are working their way through other House and Senate committees. Passage of any, alone or in some combination, is not likely for several months at the earliest. The bills in question have gathered much bipartisan support but contain differences that require some negotiation in committee rooms and lawmakers’ offices.
Throughout the whole process, APA’s Council on Psychiatry and Law and Department of Government Relations (DGR) have been closely engaged with House and Senate leadership and other parties involved in crafting the legislation, said Matthew Sturm, DGR’s deputy director. ■
The statement by Fred Osher, M.D., can be accessed here.



