Ketamine Clinics Attract Patients Despite Unknowns
Abstract
Even though ketamine is not approved by the FDA as a treatment for depression, ketamine infusion clinics are springing up in the United States as patients seek fast and effective relief.
After battling depression for years, Dennis Hartman enrolled in a clinical trial at the National Institute of Mental Health (NIMH) in 2012, where he was administered ketamine.
“It was life changing,” Hartman said of his first experience with ketamine. “I had suffered from depression for 35 years. I achieved remission within eight hours,” he told Psychiatric News.
“It was as if I had never had depression at all.”
Research Spurs Commercial Endeavors
Researchers have been trying for several years to figure out how a single dose of the anesthetic ketamine reduces symptoms of treatment-resistant depression within hours as opposed to the four to six weeks it takes most antidepressant medications to work.
Since the ketamine molecule is no longer patent protected, pharmaceutical companies have little incentive to conduct clinical trials or to seek FDA approval for its safety and effectiveness in treating depression. Nevertheless, the results of several studies demonstrating the effectiveness of ketamine in patients with treatment-resistant depression have led to a growing number of ketamine clinics.
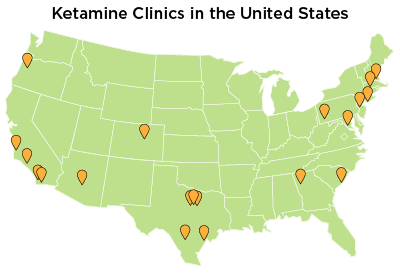
According to the Ketamine Advocacy Network, a website founded by Hartman, whose mission is to spread awareness about ketamine therapy for treatment-resistant depression, there are at least two dozen clinics around the United States that administer ketamine.
Administering ketamine to patients with depression is an off-label use of an approved drug, which is legal if performed under the supervision of a physician. Most of the current ketamine clinics in the United States are run by anesthesiologists rather than psychiatrists, likely because anesthesiologists have the most firsthand experience with using ketamine and managing side effects.
At the ketamine clinic where anesthesiologist Glen Brooks, M.D., works, patients are initially given a course of four infusions over a two-week period.
“I’ve been using ketamine for 45 years in anesthesiology,” anesthesiologist Glen Brooks, M.D., medical director of the New York Ketamine Infusions LLC told Psychiatric News. “It’s widely used in various surgeries, radiation therapy, burn units, dental anesthesia, pediatric surgery. … It’s the safest general anesthetic agent we have,” he said.
Without regulatory evaluation and approval, the ketamine dosages are generally based on published clinical studies.
“We start with 0.5 mg/kg for depression, [which was] the NIMH’s protocol,” said Kevin Nicholson, B.S.N., the chief executive officer of Ketamine Wellness Centers based in Mesa, Arizona. For anesthesia, the standard dose is 2 mg/kg.
Questions Abound for Treatment Strategies
While it works fast for many patients, approximately one-third of patients in clinical trials do not respond to ketamine.
“We need to find particular characteristics that can predict response,” APA President Maria A. Oquendo, M.D., told Psychiatric News. Oquendo is a professor of psychiatry at Columbia University, and she is involved in a randomized, controlled trial to evaluate the effectiveness and safety of ketamine in patients with refractory depression.
Even for those who respond, ketamine is not a permanent cure. In clinical trials, the effectiveness peaks around one day after the infusion and wears off over the next two weeks.
“The relief [from ketamine] lasted two weeks for me,” Hartman told Psychiatric News. “I slowly relapsed.” However, he said the experience with ketamine made a lasting impression on him. The brief freedom from depression helped him realize that he was not doomed or “defective” and that a normal mood was possible for him. He subsequently sought additional ketamine treatment after exiting the trial.

Maria A. Oquendo, M.D., says that a number of patients respond to antidepressants after exposure to ketamine.
Long-term, repeated ketamine treatment remains an area of uncertainty, as data on effective maintenance treatment are lacking.
At the New York ketamine clinic, patients are initially given a course of four infusions within approximately two weeks and can get additional infusions if they relapse. Such procedures can be expensive, with most clinics charging $400 to $800 per infusion and some even more, according to Hartman’s data. The procedure is predominantly paid out of pocket, since ketamine infusions for depression are not covered by health insurance.
Johnson and Johnson is conducting clinical trials on esketamine, an isomer of ketamine, for the treatment of treatment-resistant depression, particularly for those at imminent risk of suicide. The investigational drug is delivered through intranasal spray. If approved by the FDA, esketamine may be covered by insurance and become a more accessible treatment option.
“We have given over 4,000 infusions over the past five years,” said anesthesiologist Mark Murphy, M.D., the medical director of the Arizona clinic. The Arizona clinic follows a similar initial treatment regimen to the New York clinic. “Many patients require re-treatment every three to six months,” he added.
According to Brooks, there are patients at the New York clinic who he said have been receiving infusions for up to four years.
In some cases, patients who have responded to ketamine may do well on conventional antidepressants for maintenance, Oquendo said. In the Columbia University trial, after the initial one or two doses of ketamine, patients are offered treatment with other antidepressants.
“You’d be amazed how many patients do respond to antidepressants after ketamine,” she said.
Screening and Monitoring for Safety
The safety profile of short-term use of ketamine is well established in anesthesia. One of the most common side effects is “emergence reaction,” which occurs in about 12 percent of patients. It varies from dreamlike states to hallucination and delirium. At the lower doses for depression, dissociation—a state often described as an “out of body” sensation—is often reported.
“Hallucination and dissociation are routine for ketamine infusion,” said Murphy. Some research data and anecdotes suggest that those who experience dissociation and hallucination are more likely to reach symptom relief, although the link is still unclear. “I don’t consider them side effects [but rather] pharmacological effects of the drug.”
Besides refractory depression, ketamine has been used to treat posttraumatic stress disorder, bipolar depression, and certain types of neuropathic pain, particularly complex regional pain syndrome. Murphy estimated that 40 percent of the clinic’s patients are getting ketamine for pain and require higher doses than depression patients.
Ketamine is a Schedule III controlled substance, according to the Drug Enforcement Administration’s classification, and is known to be abused as a street drug at very high doses. The potential for abuse and addiction remains a definite concern, but evidence is limited as to what factors might increase a patient’s risk of addiction. “Careful screening of patient history for substance abuse is very important,” said Oquendo.
Brooks and Murphy emphasized that their patients undergo mental health screening before receiving ketamine infusion and have no access to ketamine outside of the clinic. They said they also recommend patients at the clinic receive ongoing psychiatric or psychological care.
“We are adamant about having strong collaboration with psychiatry,” said Murphy. The clinic employs a clinical psychologist to evaluate patients and routinely communicates with referring psychiatrists.
Because much remains unknown about the long-term effects of ketamine, Oquendo recommends that patients with treatment-resistant depression first try electroconvulsive therapy (ECT) before using ketamine, as the efficacy and safety of ECT are more well known. ■



