Psychiatrists Go Beyond Call of Duty to Respond to Harvey’s Victims
Abstract
A storm of historic proportions has engendered a nearly universal willingness among the psychiatric community to go the second mile. “One resident said, “My house is surrounded by water. But can I kayak in?”
A 6-year-old boy tries to comprehend that his stuffed animals and other toys are gone, that everything under the cots on which he and his family sleep in the George R. Brown Convention Center in hurricane-ravished Houston are all that they now own.

“What stands out in my mind are kids that you have to help to understand that there is no house to go back to,” Dakota Carter, M.D., a child psychiatry fellow at the University of Texas, told Psychiatric News.
It’s one of the countless examples of the toll that Hurricane Harvey and the record-breaking floods have taken on Houston’s citizens. At the convention center in downtown Houston and the NRG Center eight miles away (in a convention site next to the NRG Stadium, home of the Houston Texans), thousands of displaced families were sheltered as water flooded numerous neighborhoods.
In makeshift “clinics” and in cot-side visits at both sites, faculty, residents, and fellows from nearby Baylor College of Medicine and the University of Texas Health Science Center at Houston and psychiatrists in the community from the Texas district branch of APA (Texas Society of Psychiatric Physicians, TSPP) and the Harris County Medical Society (HCMS) volunteered to treat hundreds of evacuees, taking time away from their own practices and often spending days and nights at one of the two shelters. In some cases, their own homes were flooded or the roads back to them were impassable.
They offered psychological first-aid, psychotherapy, and, when needed, medication refills; a handful of individuals have been admitted to the nearby hospitals that remained open. APA’s Committee on Psychiatric Dimensions of Disaster provided psychiatrists on the ground with valuable information about psychological first-aid and other aspects of responding to a natural disaster (see sidebar).
APA Offers Help District Branches Affected by Storms
APA has offered assistance to the Texas, Florida, and Puerto Rico district branches as well as psychiatrists working on the ground to treat evacuees and others affected by hurricanes in those areas. Hurricane Maria devastated large areas of Puerto Rico on September 20 and 21; Psychiatric News will report on events there as news becomes available.
Joshua Morganstein, M.D., a member of APA’s Committee on Psychiatric Dimensions of Disaster, said that the committee—utilizing resources developed by the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences—is providing toolkits and informational resources about psychological first-aid to district branches and Assembly representatives and to psychiatrists volunteering in those areas.
He added that the committee has also developed an outreach page with resources to support response and recovery efforts related to the earthquakes in Mexico on September 9 and September 19. “This is being sent to leadership at the National Hispanic Medical Association, American Society of Hispanic Psychiatrists, APA Assembly Hispanic Psychiatrists Caucus, and Mexican Psychiatric Association.”
The APA Foundation has created a fund to provide services to those impacted by disasters. Additionally, district branches and state associations impacted by a major event are eligible for up to $10,000 from the Lindemann Disaster Fund, developed especially for disaster relief by the APA Board of Trustees.
In an email sent to APA members on September 7, APA President Anita Everett, M.D., and APA CEO and Medical Director Saul Levin, M.D., M.P.A., wrote, “We know from previous natural disasters that those affected have multiple service needs, even months and years after the traumatic event. We also know that addressing the mental health of victims, families, and communities is important. Using a social determinants of mental health model as a first step, we feel it is a priority to help people secure safety, housing and shelter, and food and water.”
Levin and Everett urged members interested in volunteering to contact the American Red Cross, which is recruiting health care professionals. They also noted that Texas Gov. Greg Abbott temporarily suspended certain rules and statutes so that health care providers licensed and in good standing in another state can assist with response to Harvey. Levin and Everett said others seeking to contribute to local charities may want to consider the Houston Food Bank or the Food Bank of Corpus Christi.
Contributions to the APA Foundation disaster fund may be made here. APA’s educational resources about responding to natural disasters can be accessed here. The website of the Houston Food Bank is available here. The website of the Food Bank of Corpus Christi is located here.
The storm dumped more than 40 inches of rain on eastern Texas in four days, followed by catastrophic flooding that inundated hundreds of thousands of homes. Some 70 deaths in Texas have been attributed to the hurricane and the floods. Recovery in the city of Houston is expected to last many months if not years.
Despite such calamity, psychiatrists who volunteered their time at both shelters uniformly reported that the hurricane and its aftermath have engendered a nearly universal feeling of connectedness among Houstonians and compelled many psychiatrists to go the second mile.
“Extraordinary selflessness” is how George Santos, M.D., past president of the TSPP and president-elect of the HCMS, who directed psychiatric services at the NRG Center, described the work of psychiatrists at the shelter. He said many have “donated enormous amounts of time, often away from their own practices.”
That sentiment was echoed by Asim Shah, M.D., a professor and executive vice chair of psychiatry at Baylor College of Medicine, who led the team at the convention center.
“This hurricane was such a sad and catastrophic event, but I can say with absolute certainty that it has brought Houston together, and it has brought the faculty and staff at Baylor together as a team and family,” Shah told Psychiatric News. He especially credited Sophia Banu, M.D., an assistant professor of psychiatry at Baylor. Shah described her as a “rock star” who was at the convention center from day one.
“When I asked people to volunteer, they just poured in. I had a resident who couldn’t go back to her house and worked 26 hours straight without complaint. Another resident couldn’t go home for three days. One resident said to me, ‘My house is surrounded by water, but can I kayak in?’ “There is story after story just like this.”
Acute Grief, Anxiety Predominant
In the first days of the storm, the convention center was a temporary home to more than 10,000 displaced Houston citizens, while the NRG center sheltered over 3,000. Ownership of the two structures dictated a rough division of labor: the shelter at the convention center, owned by the city, was run by the American Red Cross with medical and psychiatric services provided by physicians from Baylor and UT-Houston; at the NRG Center, owned by Harris County, medical and psychiatric services were provided by Harris County Health System and by the HCMS. Shah and the team at Baylor and UT-Houston also delivered services at the NRG Center before care was turned over to Harris County Health System and HCMS.
Picture a hall that is two-and-a-half football fields in length partitioned by curtains into large “dorms” or spaces lined with cots—that was the scene at the convention center. The psychiatric clinic, staffed by physicians from Baylor and UT, occupied its own curtained space.
Floridians Head Home After Irma and Mass Evacuation
As Psychiatric News went to press, residents of Florida and the Florida psychiatric community, as well as those of Puerto Rico, were just emerging from the wreckage wrought by hurricanes Irma and Maria. Many questions remained about the extent of the damage and the amount and kinds of assistance that would be needed.
Speaking to Psychiatric News on September 14, six days after the eye of Irma mowed through the Florida Keys and five days after blowing through Naples, Margo Adams, executive director of the Florida Psychiatric Society, said many Floridians were only just returning to their homes after what may have been the largest mass evacuation in American history. Nearly 7 million residents were told to leave as the storm approached.
“Trying to figure out what kind of response is necessary and what we will be asked to do is difficult,” Adams said. “This storm was huge, covering every part of the state, and capricious. There is just precious little statewide information.”
More information about the psychiatric response to Irma will appear in future issues of Psychiatric News as it becomes available.
“We started with two psychiatrists,” said Shah. “At the height of the crisis, we were up to 10 psychiatrists, including residents and fellows. Commercial pharmacies were set up within a couple of days, and we were able to refill medications. Mostly what we were seeing was acute grief, depression, and acute anxiety.”
The scene was similar at the NRG Center. “What we were tasked to do is to set up a disaster psychiatry clinic providing psychological first-aid focused on critical needs,” Santos told Psychiatric News. “But an important part of our effort was outreach—going through the ‘dorms’ and seeking out people actively in distress, then bringing them back to the clinic.”
Psychological first-aid means practical, concrete help for immediate needs, including strategies for individuals and families to regain a sense of control over their lives. “In many cases, part of our job was to connect patients with needed long-term community-based resources for ongoing therapy and medication,” Santos said. “We collaborated with the local public mental health authority to provide on-site case managers to assist with community resource referrals.”
He also credited local psychiatrists Cheryl Person, M.D., and Andrew Harper, M.D., for their part in these efforts.
Teams at both sites collaborated with the local VA to coordinate services for veterans with complications from preexisting PTSD. “I found that some of the support staff of law enforcement officers and even NRG Center staff came by to discuss their own symptoms and coping needs,” Santos said. “This comprehensive and immediate needs approach was effective and quite rewarding.”
At both shelters, a common—and heartbreaking—encounter was with children uprooted from everything they knew. Some of them were further traumatized by the storm’s television coverage, which they could watch in the shelters. For some parents who had left New Orleans after Katrina and settled in Houston, the hurricane was a matter of reliving a nightmare.
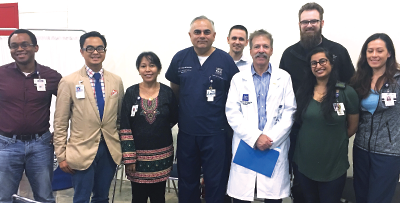
The team of psychiatrists from Baylor College of Medicine who worked at the George R. Brown Convention Center included (from left) John Saunders, M.D., John Fermo, M.D., Sophia Banu, M.D., Asim Shah, M.D., Mark Yurewicz, M.D. (in the back), Wayne Goodman, M.D., Samuel Scott, M.D. (in the back), Shana Cosha, M.D., and Suzette Toombs, M.D.
“A lot of the work we did was with traumatized parents, helping them to a be a support to their own children,” said Dakota Carter, M.D., the child fellow at UT and also the 2017-2018 APA/APA Foundation/SAMHSA/Diversity Leadership Fellow.
‘No One Complained’
By the end of the second week of September, evacuees at both the convention center and the NRG Center were rapidly transitioning back to their homes (or to the homes of friends or extended family), to hotel rooms provided by the Federal Emergency Management Agency, or to shelters in the city, and the medical and psychiatric clinics at NRG were poised to close.
For the entire population of Houston, the hurricane was an overwhelming experience. For psychiatrists and other physicians who stepped up to the call at the two shelters, it is one that will be recalled long after the waters recede.
“We all take an oath as physicians to serve humanity, but there are few moments in our professional lives when we are truly tested to live up to it,” Shah said. “For all of us, Harvey was one of those moments. A lot of us were working 12 hours or more, often with only a bottle of water or a cup of coffee. In fact, no one complained, and there was for all of us a sense of joy in what we were doing that will be hard to match.” ■
Coverage of the hurricane’s aftermath will continue as more information becomes available.



