Journal Digest
PTSD, Trauma May Increase Lupus Risk in Women

Trauma exposure and/or posttraumatic stress disorder (PTSD) may increase the risk of the autoimmune disorder systemic lupus erythematosus in women, according to a study in Arthritis & Rheumatology.
This longitudinal analysis involved 54,763 civilian women who were tracked over 24 years, during which time 73 cases of lupus occurred. Compared with women with no trauma, women with trauma exposure had a 2.87-fold increased risk of lupus, while women with probable PTSD (four to seven symptoms using DSM-IV criteria) had a 2.94-fold increased risk. There was no significant association between lupus risk and subclinical PTSD (one to three symptoms).
“We were surprised that exposure to trauma was so strongly associated with risk of lupus—trauma was a stronger predictor of developing lupus than smoking,” said lead author Andrea Roberts, Ph.D., of the Harvard T. H. Chan School of Public Health in a press release. “Our results add to considerable scientific evidence that our mental health substantially affects our physical health, making access to mental health care even more urgent.”
Roberts A, Malspeis S, Kubzansky L, et al. Association of Trauma and Posttraumatic Stress Disorder With Incident Systemic Lupus Erythematosus (SLE) in a Longitudinal Cohort of Women. Arthritis Rheumatol. September 20, 2017. [Epub ahead of print]
Changes in Personality Likely Not a Sign of Impending Dementia

Changes in personality or behavior are one of several criteria used to diagnosis dementia, but it is unclear if these changes occur prior to dementia or because of it.
A longitudinal study of more than 2,000 older adults found no evidence that personality changes occur before the onset of cognitive problems. The study did, however, find evidence to suggest that some personality traits may be greater risk factors for Alzheimer’s than others. The findings were published in JAMA Psychiatry.
The joint research team from Florida State University and the National Institute on Aging examined data from participants in the Baltimore Longitudinal Study of Aging. As part of the study, participants regularly took a personality questionnaire that assessed traits like neuroticism, extraversion, openness, agreeableness, and conscientiousness.
During the 36-year study period, 104 of the participants were diagnosed with mild cognitive impairment (MCI), and 255 with Alzheimer’s or other dementia. The investigators found that the trajectory of personality traits among people who later developed dementia or MCI did not significantly differ from non-impaired adults.
However, adults who subsequently developed Alzheimer’s had higher average scores for neuroticism and lower scores on conscientiousness than adults with no cognitive impairment.
“From a clinical perspective, these findings suggest that tracking change in self-rated personality as an early indicator of dementia is unlikely to be fruitful, while a single assessment provides reliable information on the personality traits that increase resilience … or vulnerability … to clinical dementia,” the authors wrote.
Terracciano A, An Y, Sutin A, et al. Personality Change in the Preclinical Phase of Alzheimer Disease. JAMA Psychiatry. September 20, 2017. [Epub ahead of print]
Errors in Perception Associated With Delusional Ideation

People who are prone to mistake their ability to predict outcomes also harbor more delusion-like beliefs, reports a study in Proceedings of the National Academy of Sciences. These findings point to a connection between mistimed perception and delusion, which may help diagnose or treat some mental illnesses.
Researchers at Yale University used crowdsourcing to enroll 1,013 participants to complete two related tasks. The first task asked participants to predict which of five empty squares on a screen would light up red. The researchers varied the amount of time the participants had to make this prediction. They then had to indicate whether they had made the right prediction, wrong prediction, or no prediction. For the second task, participants were asked to indicate whether a square flashing red was preceded or followed by the screen briefly going blank.
After completing their tasks, the participants all took the Peters Delusion Inventory (PDI), which measures proneness to a range of delusion-like behaviors like paranoia or magical thinking.
Participants with more “postdictions” (prediction was made after the square already flashed red, but they believed they made the prediction first) tended to score higher on the PDI. These participants performed well in the time-discrimination task, so their bias problems were not due to temporal perception but rather how they perceive prediction.
Bear A, Fortgang R, Bronstein M, Cannon T. Mistiming of Thought and Perception Predicts Delusionality. Proc Natl Acad Sci USA. September 18, 2017. [Epub ahead of print]
Ventral Striatum Activity May Protect Against Sleep-Related Depression
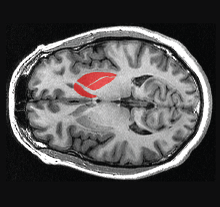
Sleep problems are a risk factor for depression, but not everyone with poor sleep develops depressive symptoms. A study by researchers at Duke University suggests increased activity in the ventral striatum—a brain region that is part of the reward system—may protect some people from sleep-related depression.
The researchers examined data from 1,129 college students who self-reported their sleep quality and depressive symptoms.The students also had MRI scans taken while engaging in a reward-based task known to activate the ventral striatum. The task involved guessing the value of a card and then receiving feedback on whether they were right or wrong.
They found that participants who displayed higher ventral striatum activity in response to positive feedback versus negative feedback were less likely to report depression symptoms despite having poor sleep.
“It is almost like this reward system gives you a deeper reserve,” senior author Ahmad Hariri, Ph.D., said in a press release. “Poor sleep is not good, but you may have other experiences during your life that are positive. And the more responsive you are to those positive experiences, the less vulnerable you may be to the depressive effects of poor sleep.”
Avinun R, Nevo A, Knodt A, et al. Reward-Related Ventral Striatum Activity Buffers Against the Experience of Depressive Symptoms Associated With Sleep Disturbances. J Neurosci. September 18, 2017. [Epub ahead of print]
Schizophrenia Mortality Gap Is Widening

The longevity gap between the overall population and people with schizophrenia appears to be widening, reports a meta-analysis published in Schizophrenia Research.
Investigators at the University of California San Diego School of Medicine compiled data from eight population studies of schizophrenia patients. They found that the mean standardized mortality ratio (SMR) for schizophrenia (the ratio of observed deaths in a certain group to expected deaths in the general population) has been rising since the 1970s.
The average SMR has increased from 2.2 to 3.0 (increase of 37 percent)—meaning that there are three times as many deaths among people with schizophrenia as should be expected. Only two of the studies included in the meta-analysis provided details on the cause of death, but both showed that the SMR for unnatural deaths such as suicide has remained stable, while the SMR for natural deaths has risen.
“It is likely that these findings reflect on persistent and pervasive stigma against mental illness and societal neglect of this vital yet vulnerable segment of the population, which continues to be disenfranchised,” the study authors wrote. ■
Lee E, Liu J, Tu X, et al. A Widening Longevi-ty Gap Between People With Schizophrenia and General Population: A Literature Review and Call for Action. Schizophrenia Res. September 27, 2017. [Epub ahead of print]



