Syrian Refugees: Crisis Beyond Borders
Abstract
An ongoing, long-term need for mental health services is emerging for the 4.8 million Syrians driven from their country.
The recent fall of Aleppo to Syrian government forces again brought to the forefront the dire situation of refugees from that conflict and others in the region.

The bucolic painting on the caravan stands in contrast to the desert environs of the Zaatari Camp in northern Jordan. The camp opened in 2012 and now houses about 80,000 Syrian refugees.
Half of Syria’s 24 million people have been uprooted from their homes by the six-year-old, multisided civil war. An estimated 4.8 million Syrians have fled their country, most to nearby Turkey, Jordan, Lebanon, Iraq, and Egypt. Some have managed to move farther on, through Greece to northern Europe and the United States. All have been traumatized to some degree by a combination of oppression, displacement, and an uncertain future.
For most refugees, once they left Syria, the necessities of life—safety, shelter, clothing, food—came first. However, the inevitable psychological stressors eventually require care as well.
Some of that work has taken place inside Syria, even during a brutal war, said Yassar Kanawati, M.D., a Syrian-American psychiatrist in private practice in Atlanta and a volunteer with the Syrian American Medical Society (SAMS).
From outside the country, SAMS has supported clinics in several Syrian cities. One, in the besieged Damascus suburb of Ghouta, serves mainly women and children, since many men there have been killed, detained, or simply disappeared.
“The clinic also tries to find educated women to provide some schooling for children,” said Kanawati in an interview. “Mothers can also get some individual or group therapy.”
She has visited refugee camps in Jordan and Turkey several times to help with difficult cases, which she then follows using Skype or other web-based communications to consult with local clinicians.
The International Rescue Committee (IRC) also manages medical teams within Syria from locations in Jordan and Turkey by providing salaries, training, supervision, medications, and supplies, said Ashley Nemiro, Ph.D., IRC’s technical advisor for mental health.
The IRC and other nongovernmental organizations provide care in Lebanon, Jordan, Turkey, and Iraq to refugees once they have left Syria.
In refugee camps in northeast Syria, IRC is incorporating mental health services in general medical clinics. There, IRC sends caseworkers to deliver a 10-session strategy on caring for loved ones who are caring for the elderly or individuals with disabilities or mental health concerns while maintaining the caregiver’s (usually women) mental health, said Nemiro.
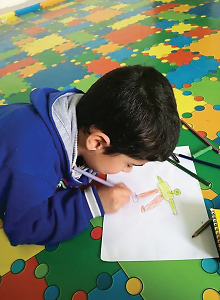
Children like this refugee boy in Irbid, Jordan, can receive individual, group, or play therapy in programs run by the Syrian-American Medical Society.
Social workers and psychologists provide psychosocial interventions, primarily to women and children because of the increased stress they face after husbands and fathers have been killed or have left for Europe to find work and escape military recruitment, she said.
Due to the recent fighting around Mosul in Iraq, IRC has sought to fill a critical gap by providing male Iraqi refugees with tailored mental health interventions. Men in the camps can learn about nonviolent communication to deal with the anger and frustration engendered by their displacement and loss of work, as well as the aftermath of extreme violence and torture while they were under ISIS control.
“It’s our responsibility to provide a space where men can address these wounds,” she said.
IRC prefers to employ local mental health professionals who already know the language of their clients and understand the refugees’ cultural context and their idioms of distress, said Nemiro.
Another organization, the International Medical Corps, had set up an office in Damascus before the civil war began to serve refugees from the fighting in Iraq, but it currently serves displaced Syrians. The organization hires local staff in Lebanon and Jordan to provide services to refugees from Syria, but in Turkey, Syrian providers are used because they can obtain work permits there, said Claire Whitney, M.I.A., L.C.S.W., the International Medical Corps’ regional mental health and psychosocial services advisor for the Middle East.
Refugees may present with varying kinds of psychosocial and psychiatric distress, mostly depression and anxiety, she said in an interview. “Symptoms of preexisting mental diagnoses often are exacerbated by displacement, so we try to identify individuals with those conditions and their families to get them help.”
Help can come on several levels. Psychoeducation and peer-to-peer support groups are available. Services for individuals are provided by psychosocial workers, with referral to host-country or International Medical Corps psychologists and psychiatrists when available.
“Individual care still has to involve family and community supports, much more so than in the West,” said Whitney.
European countries are also coping with the waves of migrants. Applications for asylum in Sweden alone totaled 162,000 in 2015; that number dropped to a still substantial 27,000 in 2016 as borders closed and restrictions increased, said psychologist Gaia Quaranta, M.A., a mental health activity manager for Mȳdicins Sans FrontiȲres/Doctors Without Borders (MSF) in GɆtene, where there are two reception centers for refugees.
One center is managed by the Red Cross for victims of torture. There is now a one-month wait for assessment and a one-year wait for treatment.
MSF personnel work outside the reception centers, she said in an interview. “We screen to decide whether they need specialized help and then refer to the local primary health care system, but MSF does not provide direct mental health care.”
MSF does have three counselors in GɆtene, plus four cultural mediators who speak Arabic, Farsi, or Dari, she said. “Our goal is to bring out resilience and offer psychosocial support so the refugees don’t get worse.”
The recent wave of refugees has begun to overwhelm the patience and hospitality of European and other nations. Recent changes in the Swedish asylum process are just one example. Refugees can apply only for temporary, three-year residency permits now but may wait a year before hearing a decision on their status, said Quaranta. “So people stay in the reception centers for a long time, and it’s quite stressful on top of the traumatic experiences in their home countries and on their journeys.”
The United States has received relatively few refugees from Syria and other conflict zones. The IRC has tracked 3,138 individuals across its network in this country, including 649 Syrians, said Nemiro. The organization screens all its clients for anxiety, depression, and PTSD and refers them to outside mental health specialists when needed. It also offers a group-based “Pathways to Wellness” program to help refugees cope with the stresses of resettlement.
Some refugees have faced more extreme stresses than others. Mayada Akil, M.D., a professor of psychiatry and vice chair for education at Georgetown School of Medicine, works with asylum seekers in the Washington, D.C., area from the Middle East, Africa, and other areas, especially those who have survived torture.
Symptomatic presentation varies widely, said Akil, who was born in Syria and still has family there.
“They have already experienced trauma and displacement, face an uncertain future, and remain anxious about their families back in their home countries,” said Akil. Many have symptoms but do not meet diagnostic criteria thresholds, creating some barriers to services.
“The current environment in the United States makes refugees less hopeful of getting asylum,” she said. “The process is slow and bogged down, and we don’t know what will happen in the future.”
Akil would like to see greater involvement in recruiting resources for refugee care on the part of APA and its members.
For some, a telepsychiatry model employed by the Syrian American Medical Society may represent one opportunity. Kanawati works remotely over the Internet, consulting nurses and social workers on the ground and occasionally doing therapy.
“Visiting refugee camps is not a long-term solution,” said Akil. “Psychiatry is not like surgery. You can’t do treatment in a week’s visit.”
At present, prospects for any early safe return for the refugees seem dim, said Whitney. “Nobody expected the war to last this long, so people are finally realizing that this is not temporary.”
“Things are getting worse,” agreed Kanawati. “We are now trying to develop community mental health programs in the surrounding countries for the long term.” ■
For more information: Syrian American Medical Society; International Rescue Committee; and International Medical Corps. More about Doctors Without Borders/Mȳdecins Sans FrontiȲres (MSF)’s work in Syria can be accessed here.



