Journal Digest
Gout, Malaria Medications Reduce Opioid Withdrawal in Rodents

The anti-gout medication probenecid and the antimalarial mefloquine may help to alleviate symptoms of opioid withdrawal, according to a recent animal study by researchers at the University of Calgary. The medications act on the pannexin-1 (Panx1) channel—which the researchers determined plays a key role in morphine withdrawal.
While previous research on withdrawal has focused on the spinal cord itself, the investigators in this work observed that microglia—the resident immune cells of the central nervous system—around the spinal cord were facilitating some of the nerve changes brought on by the withdrawal.
Subsequent genetic knockout studies identified the Panx1 gene as a key regulator of this microglial function.
When the investigators treated rodents with the clinically used Panx1 blockers probenecid and mefloquine they found the medications alleviated the severity of withdrawal.
“Opioids are the pharmacological cornerstone for treating chronic pain in a large variety of diseases,” said study author Tuan Trang, Ph.D., in a statement. “Understanding why opioid withdrawal occurs and how to alleviate it is of critical importance in improving pain therapy and may have implications for substance abuse.”
This study was published in Nature Medicine.
Burma N, Bonin R, Leduc-Pessah H, et al. Blocking Microglial Pannexin-1 Channels Alleviates Morphine Withdrawal in Rodents. Nat Med. January 30, 2017. [Epub ahead of print]
Brain Scans May Predict Future Depression, Anxiety
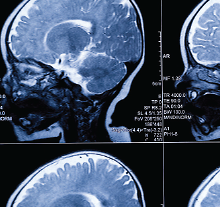
Internalizing symptoms in children, such as extreme shyness or separation anxiety, are known to be indicators of future depression or anxiety disorders. A study in the Journal of the American Academy of Child and Adolescent Psychiatry now suggests that these differences may be evident in the brains of infants who are just a few days old.
Researchers used functional magnetic resonance imaging (fMRI) to take brain scans of newborns (65 full term and 57 preterm) and map out the strength and pattern of neural connections between the amygdala (a key region involved with processing emotions) and other parts of the brain.
When these babies reached two years of age, a subset (17 full term and 27 preterm) received psychological assessments, which evaluated internalizing symptoms including as general anxiety and separation distress. Such symptoms have been linked with an increased risk of clinical depression and anxiety disorders in older children.
When comparing the infant brain scans with the toddler assessments, the authors found certain connectivity patterns between the amygdala and the insula or prefrontal cortex (brain regions that are affected in depression and generalized anxiety in adults, respectively) were associated with greater internalizing symptoms at age two. These patterns were present in both full-term and preterm infants; the latter simply had weaker amygdala connections. Despite these differences, full-term and preterm infants had the same prevalence of internalizing symptoms at age two.
“These results suggest that the seeds of future anxious and depressive symptoms for some individuals may be detectable at birth using amygdala connectivity patterns,” the authors wrote.
Rogers C, Sylvester C, Mintz C, et al. Neonatal Amygdala Functional Connectivity at Rest in Healthy and Preterm Infants and Early Internalizing Symptoms. J Am Acad Child Adolesc Psychiatry. February 2017; 56(2):157-166.
Cosmetic Professionals Know About BDD, But May Miss Signs

While cosmetic professionals have some awareness of body dysmorphic disorder (BDD) and the challenges it poses, they may be under-diagnosing the condition, reports a survey study published in Plastic and Reconstructive Surgery.
The findings were based on the feedback of 173 cosmetic professionals in The Netherlands, who completed an online survey that inquired about knowledge of and interactions with patients with BDD.
Most of the professionals surveyed said they were familiar with BDD and its diagnostic criteria and had encountered BDD patients in their clinics. Approximately 70 percent of the respondents also said they had refused to perform cosmetic procedures in a patient they suspected of having BDD.
However, based on the professionals’ estimates, only about 2 percent of patients going to their clinics had BDD, whereas other studies have estimated that up to 10 percent of people who go to cosmetic clinics have BDD.
“Ideally, cosmetic professionals should be explicitly educated about recognizing and managing psychological contraindications during their clinical training, just as they are informed about numerous somatic contraindications,” the study authors wrote. “This would make the exploration of body image problems a standard topic in every patient encounter in a cosmetic clinic.”
Bouman T, Mulkens S, van der Lei B. Cosmetic Professionals’ Awareness of Body Dysmorphic Disorder. Plast Reconstr Surg. February 2017; 139(2):336-342.
Bilingualism May Help Brain Compensate for Neurodegeneration

Recent studies have suggested that lifelong bilingualism may help delay the onset of dementia, but the underlying neural mechanism of this potential protective effect is unknown.
A study in Proceedings of the National Academy of Sciences found that people who speak two languages may have stronger neural connections that allow them to compensate for neurodegeneration in other regions of the brain.
A total of 85 patients (45 German-Italian bilingual speakers and 40 monolingual speakers) with probable Alzheimer’s disease (AD) underwent positron emission tomography (PET) scanning.
The scans showed that even though bilingual individuals with AD had stronger metabolic deficiencies in some brain regions than monolingual individuals, they outperformed monolinguals on verbal memory and visual-spatial tasks. Bilingual patients also had stronger neural connections between the anterior and posterior brain regions than those who spoke one language only.
“Overall, these findings strongly suggest that bilingual individuals with AD compensate better for the loss of brain structure and function,” the authors wrote.
Perani D, Farsad M, Ballarini T, et al. The Impact of Bilingualism on Brain Reserve and Metabolic Connectivity in Alzheimer’s Dementia. Proc Natl Acad Sci USA. January 30, 2017 [Epub ahead of print]
Crisis-Response Plans Found to Cut Suicidal Behavior in Military

Crisis-response planning can be effective in reducing suicidal behavior in military personnel, reports the Journal of Affective Disorders.
The findings come from a randomized study of 97 active service military who had sought help for suicidal ideation or attempt at an emergency behavioral health clinic. The participants were divided to receive one of three risk management strategies: a contract for safety in which a patient provides a commitment to avoid self-harm; a standard crisis-response plan, which involves writing down how to identify suicidal warning signs as well as coping strategies or support services that can be used in a crisis; or an enhanced crisis-response plan in which patients write down all of their reasons for living in addition to the other elements of the plan.
The patients were followed for six months. Those who received crisis-response planning reported a faster decline in suicidal thoughts than those who received a contract for safety. The number of inpatient hospitalizations were also lower in patients who received the crisis planning.
Crisis-response planning also resulted in a 75 percent reduction in suicide attempts, though the total numbers were small (three attempts among the two crisis-plan groups and five attempts in the contract-for-safety group).
There were no significant differences between patients in the two crisis-response-plan groups.
Bryan C, Mintz J, Clemans T, et al. Effect of Crisis-Response Planning vs. Contracts for Safety on Suicide Risk in U.S. Army Soldiers: A Randomized Clinical Trial. J Affect Disord. January 23, 2017; 212:64-72.
Alcohol Abuse Increases Risk of Cardiovascular Problems

Alcohol abuse increases the risk of atrial fibrillation, heart attack, and congestive heart failure to an extent similar to that of other well-known cardiovascular risk factors, reported a study published in the Journal of the American College of Cardiology.
The findings come from an analysis of data from nearly 15 million adult California residents who received ambulatory, emergency, or inpatient care in California between 2005 and 2009. The researchers quantified the occurrences of alcohol abuse, cardiovascular outcomes, and other health data using International Classification of Diseases-9th Revision (ICD-9) and Current Procedural Terminology (CPT) codes given for each patient visit.
After adjusting for other potential risk factors, a diagnosis of alcohol abuse was associated with a 2.14-fold increased risk of atrial fibrillation, a 1.45-fold increased risk of heart attack, and a 2.34-fold increased risk of congestive heart failure. These magnitudes were on par with other well-established risk factors including male sex, smoking, obesity, hypertension, and chronic kidney disease. Among atrial fibrillation risk factors, for example, alcohol abuse was second only to congestive heart failure in terms of independent fibrillation risk.
“Although nearly all subgroups exhibited increased risk in the setting of alcohol abuse, those without a given risk factor for each outcome were disproportionately prone to enhanced cardiovascular risk.” However, while the relative risk of atrial fibrillation, heart attack, or heart failure rose significantly in this group, the absolute risk was still low, they added. ■
Whitman I, Agarwal V, Nah G, et al. Alcohol Abuse and Cardiac Disease. J Am Coll Cardiol. January 3, 2017; 69(1):13-24.



